Evaluating postoperative pain and satisfaction among women treated by robotic surgery for gynecologic cancer
Introduction
Pain has been described as among the worst and most prevalent symptoms of cancer and its treatments (1-4). Pain has also been associated with longer recovery time (5), higher postoperative readmission rates (6), and interference with patients’ daily activities, wellbeing, and enjoyment of life (3,7,8), as well as their social surroundings including family and caregivers (3,8).
Pain is a subjective feeling that may result from the activation of nociceptors by noxious stimuli such as tissue damage (e.g., surgery), and is often followed by hyperalgesia (a heightened response to noxious stimuli) and/or allodynia (a feeling of pain induced by normally non-noxious stimuli) (9). Acute pain may also have the potential to become chronic (10), sometimes persisting long after surgery and adding to the long-term morbidity and interference with daily life (9,11-15).
In spite of advancements in the field of pain management and the availability of tools to alleviate this distressing symptom, pain continues to be undermanaged in cancer patients (3,4,7,8,16,17). In many of these individuals, pain intensity is often moderate to severe (1,3,4,7).
In gynecology and gynecologic oncology, the introduction of laparoscopy has significantly reduced postoperative pain in patients in whom the technique is feasible (18,19). Robotically-assisted surgery has facilitated the practice of minimally invasive surgery, allowing an increasing number of patients to benefit from the procedure. Some groups have shown similar benefits for robotic surgery with respect to postoperative pain reduction (20,21), though studies have mostly focused on the immediate postoperative period without assessing preoperative pain or the long-term impact of surgery.
Results from our pilot study demonstrated that two thirds of patients reported feeling no pain by the first postoperative visit after robotic surgery (at three to four weeks) for the treatment of endometrial cancer (22). Limitations of our pilot study included the lack of a preoperative baseline questionnaire and the use of a questionnaire that had not been validated (22). In the current study, we address these limitations to better describe the short- and long-term impact of robotic surgery on pain and its interference with daily life in women treated for gynecologic cancer. The secondary objective is to describe patients’ satisfaction with their surgery.
Methods
All consecutive patients planning to undergo robotic surgery for the treatment of a suspected gynecologic cancer between December 2009 and December 2012 were invited to participate in this prospective study (23). During the preoperative clinic visit, participants were given an informed consent form and a questionnaire assessing baseline self-reported outcomes including levels of pain. Postoperative questionnaires were handed or mailed to participants in the short term (one week and three weeks) and long term (three, six, and twelve months) after surgery. Patients were excluded if their surgery was converted to laparotomy (n=14) or if they were re-operated by laparotomy prior to being discharged from the hospital (n=1).
Pain was evaluated using the brief pain inventory (BPI) (24,25). This validated questionnaire asks if participants feel pain “other than everyday kinds of pain” and if they are taking any treatments for their pain. Treatments for pain were categorized as no treatments, NSAIDs or Acetaminophen, opioids or opioid-containing medications (e.g., codeine, morphine, acetaminophen-codeine combination, etc.), physical therapy (e.g., massage, physiotherapy, etc.), alternative medicine (naturopathy, homeopathy, acupuncture), and/or other. The BPI asks participants to rate the pain they felt in the last 24 hours at their worst, least, on the average, and in that moment on a scale of 0 to 10 from no pain to worst imaginable pain. The four answers are averaged to give a pain severity score (24), and can be reported as mild (scores 1–4), moderate (scores 5–6), or severe (scores 7–10) (26). The BPI assesses how pain interfered, on a scale of 0 to 10, with different aspects of life: general activity, mood, walking ability, normal work, relations with other people, sleep, and enjoyment of life. Scores are averaged to give an overall pain interference score (24). Based on the guidelines (24), pain severity scores were only calculated if all four component questions were answered, and pain interference scores were only calculated if more than half of the questions were answered. To remain conservative, if participants circled more than one answer or were between two values on any of the numerical rating scales, only the worst score was counted.
Included in the postoperative questionnaires were a series of questions related to patients’ satisfaction with the surgery. Patients were asked to rate their satisfaction with their recovery time as well as with their surgery overall on a scale of 0 to 10 from not at all to completely satisfied. In addition, participants were asked to rate, on a scale of 1 to 4 from not at all to very much, to what extent the surgery met their expectations and whether they would recommend the surgery to someone in similar circumstances.
The study was approved by the Jewish General Hospital’s Research Ethics Office (protocol #09-123) and informed consent was obtained from all patients.
Statistical analysis
Responses to questionnaires were recorded on Microsoft Excel 2003, statistical analysis was performed using STATA 13 (StataCorp), and figures were produced in Excel. Pain outcomes were regressed against the timing of the questionnaires using univariate logistic and linear models as well as stepwise multiple logistic and linear regression models to control for the timing of the questionnaires, primary suspected tumor site, age (<70 vs. ≥70 years old), body mass index (BMI), marital status, and highest education level attained. For logistic regressions, odds ratios were shown as OR [95% confidence interval (CI)], and for linear regressions, beta coefficients were shown as β (95% CI). The Wilcoxon Sign Rank test and the McNemar test were used, where appropriate, to compare postoperative pain responses to baseline scores. Statistical significance was defined as P<0.05 throughout the study.
Results
Baseline characteristics
Patient demographics and lifestyle habits are shown in Table 1. Two thirds of patients (n=245, 67%) were treated for a suspected endometrial cancer on endometrial biopsy. Beginning one year after the start of our robotics program, patients with an ovarian tumor were carefully selected for robotic surgery, representing 22% of subjects in the current analysis. One hundred fifty-seven patients (43%) were obese. The mean age was 61 years old (±13 years) and 23% were elderly (70 years or older). More than half of patients (56%) reported a college or university degree. Most patients reported being in a relationship (64%), and the majority (78%) had children.
Table 1
| Characters | n (N=367) (%) |
|---|---|
| Suspected or confirmed tumor site | |
| Uterus | 245 (67%) |
| Ovaries, fallopian tubes, peritoneum | 79 (22%) |
| Cervix | 43 (12%) |
| BMI | |
| <30 | 210 (57%) |
| 30.0–39.9 | 105 (29%) |
| ≥40 | 52 (14%) |
| Highest education level* | |
| Elementary | 27 (7%) |
| Secondary | 112 (31%) |
| College/university | 205 (56%) |
| No answer | 23 (6%) |
| Current relationship status | |
| Married | 198 (54%) |
| Cohabitating | 26 (7%) |
| Dating | 12 (3%) |
| Single, widowed, divorced | 118 (32%) |
| No answer | 13 (4%) |
| Children | |
| Yes | 287 (78%) |
| No | 27 (7%) |
| No answer | 53 (14%) |
| Alcohol drinking habits | |
| None | 154 (42%) |
| Occasionally | 69 (19%) |
| 1–3/week | 57 (16%) |
| ≥4/week | 62 (17%) |
| No answer | 25 (7%) |
| Cigarette consumption | |
| None | 316 (86%) |
| Very few or rarely | 1 (0%) |
| 1–5/day | 7 (2%) |
| 6–10/day | 8 (2%) |
| >10/day | 14 (4%) |
| No answer | 21 (6%) |
| Exercising habits | |
| Never | 135 (37%) |
| ≤5 times per month | 8 (2%) |
| 1–4 times per week | 124 (34%) |
| ≥5 times per week | 68 (19%) |
| No answer | 32 (9%) |
*, subjects who only reported years of schooling were categorized accordingly.
General pain & treatments for pain
The first item on the BPI asks whether patients have any pain other than “everyday kinds of pain”. More patients reported pain at the one-week follow-up compared to baseline (42% at baseline vs. 58% by the first week, P=0.002), and this returned to baseline within three weeks after surgery (40%, P=0.7), and remained statistically non-significant for the remaining follow-ups.
Whether or not patients reported pain was regressed against the time since surgery in a univariate analysis. At the one-week follow-up, patients were close to twice as likely to report pain [OR =1.9 (1.3–2.8), P=0.002]. By the three-week follow-up, the likelihood of patients reporting pain had already returned to baseline [OR =0.9 (0.6–1.4), P=0.6], and this was sustained until one year after surgery. As shown in Table 2, similar results were obtained after controlling for demographic and clinical factors (diagnosis, elderly status, obesity, educational status, and marital status): the likelihood of reporting pain increased by the first week [OR =2.18 (1.54–3.08), P<0.001] and returned to baseline by the second follow-up three weeks after surgery (P=0.81).
Table 2
| Predictor variables | Pain other than everyday pain* | Treatments for pain* | Pain severity† | Pain interference† | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | SE | P value | OR (95% CI) | SE | P value | β (95% CI) | SE | P value | β (95% CI) | SE | P value | ||||
| Visit | |||||||||||||||
| Before surgery | |||||||||||||||
| 1 week after surgery | 2.18 (1.54–3.08)& | 0.39& | <0.001& | 5.92 (4.12–8.50) & | 1.09& | <0.001& | 0.56 (0.23–0.90)& | 0.17& | 0.001& | 1.27 (0.90–1.65)& | 0.19& | <0.001& | |||
| 3 weeks after surgery | 0.81 | 0.69 | 0.21 | 0.65 | |||||||||||
| 3 months after surgery | 0.77 (0.54–1.09) | 0.14 | 0.14 | 0.27 | 0.75 | 0.30 | |||||||||
| 6 months after surgery | 0.69 | 0.44 | 0.99 | 0.90 | |||||||||||
| 12 months after surgery | 0.66 (0.41–1.06) | 0.16 | 0.086 | 0.80 | 0.73 | 0.86 | |||||||||
| Diagnosis | |||||||||||||||
| Endometrial | |||||||||||||||
| Ovarian | 0.85 | 0.97 | 0.41 | 0.42 | |||||||||||
| Cervical | 1.92 (1.25–2.95)& | 0.42& | 0.003& | 0.18 | 0.57 (0.15–1.00)& | 0.22& | 0.009& | 0.39 (−0.10–0.88) | 0.25 | 0.12 | |||||
| Age (years) | |||||||||||||||
| <70 | |||||||||||||||
| ≥70 | 0.72 (0.50–1.03) | 0.13 | 0.071 | 0.80 | 0.78 | 0.50 | |||||||||
| BMI | |||||||||||||||
| <30.0 | |||||||||||||||
| 30.0–39.9 | 0.34 | 0.61 | 0.69 | 0.16 | |||||||||||
| ≥40 | 0.57 | 0.41 | 0.35 (−0.075–0.78) | 0.22 | 0.11 | 0.53 (0.038–1.02)& | 0.25& | 0.035& | |||||||
| Marital status | |||||||||||||||
| Single/divorced/widowed | |||||||||||||||
| Married/dating/cohabitating | 0.76 (0.56–1.04) | 0.12 | 0.083 | 0.60 | 0.58 | 0.27 | |||||||||
| Education | |||||||||||||||
| Up to high school | |||||||||||||||
| More than high school | 0.61 (0.45–0.82)& | 0.092& | 0.001& | 0.80 (0.59–1.08) | 0.12 | 0.15 | −0.84 (−1.13–−0.55)& | 0.15& | <0.001& | −0.51 (−0.83–−0.18)& | 0.17& | 0.003& | |||
*, multiple logistic regression model showing odds ratio (OR) with 95% confidence interval (CI) and standard error (SE); †, multiple linear regression model showing beta coefficient (β) with 95% confidence interval (CI) and standard error (SE); &, significant results (P<0.05) are presented.
Patients who had more than a high school education were less likely to report pain other than everyday kinds of pain [OR =0.61 (0.45–0.82), P=0.001] and patients undergoing surgery for the diagnosis of cervical cancer were more likely to do so than those with a diagnosis of endometrial cancer [OR =1.92 (1.25–2.95), P=0.003]. The remaining factors in the model were not significant.
When asked whether or not they were taking treatments for their pain, more patients reported taking pain medications at their one-week follow up compared to baseline (73% at one week compared to 31% at baseline, P<0.0001), again returning to baseline by the three-week follow-up (33%, P=0.3).
In the univariate analysis, the use of treatments for pain was associated with the one-week follow-up [OR =5.92 (4.12–8.50), P<0.001], returning to baseline within three weeks of surgery [OR =1.1 (0.6–1.8), P=0.8]. Similar results were obtained after controlling for the aforementioned baseline variables, and none were significantly associated with whether treatments were taken for pain.
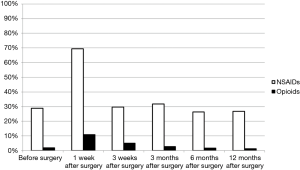
Figure 1 illustrates the types of treatments patients reported taking for pain across time points. Treatments were divided into none, NSAIDs and/or acetaminophen, and opioids. Before surgery, 69% of patients were not taking treatments for pain, 29% were using NSAIDs, and 2% took opioid-containing medications. By one week, these changed to 27%, 70%, and 11%, respectively, and returned close to baseline by three weeks: 67%, 30%, and 5%, respectively. Percentages sum up to over 100% due to overlap between those taking both NSAIDs and opioid-containing medications. Few patients (<4% at each time point) also described employing physical therapy, alternative medicine, or other means of pain management.
Pain severity & pain interference
Pain severity and interference were higher at the one-week follow-up [β =0.56 (0.23–0.90), P=0.001, and β =1.27 (0.90–1.65), P<0.001, respectively] but returned to baseline by three weeks [β =−0.2 (−0.7–0.3), P=0.21, and β =−0.3 (−0.8–0.3), P=0.65, respectively].
The stepwise linear regression analyses for pain severity and interference are tabulated in Table 2. Similar results were obtained after controlling for baseline factors: higher pain severity and interference were significantly associated with the one-week follow-up (P=0.001 for pain severity; P<0.001 for pain interference), returning to baseline by the three-week follow-up. Educational status was also a significant factor, with higher education associated with less pain severity (P<0.001) and interference (P=0.003). Patients treated for a cervical cancer were also associated with higher pain severity scores (P=0.009) while patients with morbid obesity (BMI greater than or equal to 40 kg/m2) were associated with greater pain interference (P=0.04).
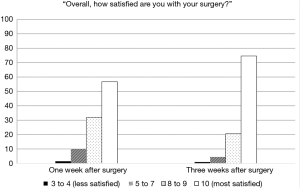
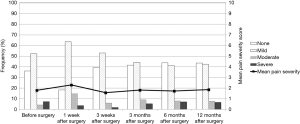
Figure 2 shows the change in mean pain severity scores over time as well as the proportions of patients reporting the different levels of pain severity (no pain, mild, moderate, or severe pain). Pain severity and pain interference scores at each postoperative time point were compared to baseline using the Wilcoxon signed rank test. Both pain severity and interference increased by the one-week follow-up (P=0.02 and P=0.0001, respectively) but returned to baseline within three weeks (P=0.6 and P=0.2).
Pain severity and pain interference were found to be strongly correlated (r=0.67, P<0.001).
Satisfaction with surgery
Patients’ overall satisfaction with their surgery at one week and at three weeks after surgery is illustrated in Figure 3. By the first week, the mean overall satisfaction score was 9.1 out of 10 (median and modal score of 10 or completely satisfied) and patients reported being satisfied with their recovery time following their surgery (mean score of 8.3; median of 9; mode of 10). By week three, the mean scores were 9.5 and 8.9, respectively, and 95% of respondents rated their overall satisfaction at 8 or higher.
Regarding whether the surgery met their expectations by the one-week follow-up, the mean score was 3.7 out of 4 (median and mode of 4 or very much). Most patients would also recommend the surgery to someone in similar circumstances with a mean score of 3.9 (median and mode of 4).
Following the first week, the median scores on the above dimensions of satisfaction were the maximum value (i.e., 10 or 4 depending on the question) for all subsequent follow-ups.
Sensitivity analysis
In order to control for variability in surgical procedures and the presence of malignancy on final pathology, the analysis was repeated after removing patients with no cancer (n=66, 18%) and/or those who did not have a hysterectomy (n=35, 10%). Similar results were obtained with pain scores returning to baseline by three weeks after surgery. Of note is that across the multivariable regression models, a diagnosis of ovarian cancer became significantly associated with increased pain scores.
Discussion
Our findings show that pain outcomes tended to increase at the first follow-up one week after robotic surgery but returned to baseline within three weeks of surgery. Even in the short term after surgery, the majority of patients were satisfied with the surgery, and did not require narcotics (89%); NSAIDs and/or acetaminophen seemed sufficient for pain control. This is consistent with our previous publication on a matched historical cohort of patients treated for endometrial cancer by laparotomy, showing that patients who underwent robotic surgery used less analgesics, including significantly less opioids, and were much less likely to be given patient-controlled analgesia in the immediate postoperative period (27).
The landmark trial LAP2 compared outcomes between laparotomy and laparoscopy for the staging of early endometrial cancer (18). The study set a precedent for laparoscopy as a less invasive approach to reduce postoperative pain, as measured using items from the BPI, with pain severity measured using worst and least pain (18). While differences in pain scores between treatment arms were compared for statistical significance, pain scores over time were not compared to baseline to measure the impact of surgery over time. Still, the magnitude of the changes in pain scores is noteworthy. We recalculated pain severity and interference scores among patients who were diagnosed with a confirmed endometrial cancer, using the same methodology as in the LAP2 study. Caution should be taken in interpreting these differences in pain scores across two different studies and study populations, however the robotic cohort presented in this manuscript exhibited an increase in pain severity of 24% from baseline to the one-week follow-up, and, by three weeks, pain severity scores were already less than pre-surgery levels (13% decrease). In contrast, pain severity more than doubled in the laparoscopy and laparotomy arms in LAP2’s intention-to-treat analysis (150% increase from baseline to one week after surgery), and were still higher at three weeks (close to 50% increase from baseline) (18). Similarly so for pain interference, our robotic cohort noted a 58% increase in pain interference from baseline to one week after surgery, reaching lower than pre-surgery levels by three weeks (6% decrease). In the LAP2 cohorts, those assigned to laparoscopy and laparotomy reported an over 200% increase in pain interference by one week after surgery, and by three weeks, pain interference scores were still over double pre-surgery levels (18).
Using the SF-36 bodily pain subscale, another study indicated worse mean bodily pain scores by the six-week follow-up in comparison to baseline in both the laparotomy and laparoscopy groups, though these were not compared to baseline for statistical significance (28). In a study combining both benign and malignant gynecologic cases (20), and in a study on benign gynecologic cases only (29), no significant differences in pain scores were observed between laparoscopy and robotic surgery.
In our sample, patients with more than a high school education were significantly less likely to report pain other than everyday kinds of pain (P=0.001) and were associated with significantly less pain severity (P<0.001) and interference with daily life (P=0.003). van den Beuken-van Everdingen et al. [2007] reported on the prevalence, severity, and adequacy of treatment for pain among patients with cancer (4). In accordance with our findings, age and marital status were not significantly associated with the prevalence of pain, while patients with lower education levels were associated with a higher risk of pain (4).
BMI was not significantly associated with patients’ reporting of pain, use of treatments for pain, or pain severity. This supports findings from our pilot study where we reported no impact of BMI on analgesic use (22). However, in the current study, a BMI of 40 kg/m2 or higher was associated with greater interference of pain with daily life. Our pilot study also demonstrated a significant impact of age on the reporting of pain after surgery with a greater proportion of younger patients reporting no pain (22). With the introduction of a baseline questionnaire in the current study, we found that elderly status was not significantly associated with any of the pain outcomes. Additionally, as in the current study, participants in our pilot analysis also reported high levels of satisfaction with the surgery (22).
Limitations of the current study include incomplete as well as missing questionnaires, a challenge of many survey-based studies (Table S1). While only few patients who completed the pain questionnaires did not provide valid assessments, the pain severity and interference analyses were repeated without excluding patients with incomplete data, and this yielded similar results. Moreover, while a validated and reliable instrument was used for the pain assessment, the satisfaction survey was not a validated questionnaire and respondents’ satisfaction could have been influenced by other aspects of their care apart from the robotic surgery. However, while capturing the patient experience has its challenges (30), we included the questions to generate feedback and to incorporate broader measures of the quality of surgical care from the patients’ perspectives. In addition, the current study focuses on patient-reported outcomes following robotic surgery; patients treated via laparotomy or laparoscopy were not included. At the time robotics was being rolled out in our division, up to 15% of all hysterectomies for a gynecologic cancer were done by laparoscopy (manuscript in submission, January 2019). Since then, rates of minimally invasive surgery reached over 90% due to the use of the robotics platform (manuscript in submission, January 2019). Another limitation is that this study was limited to a single tertiary hospital in Canada and some have reported on differences in patient-reported pain and pain management across different countries as well as ethnicities (31,32). For example, in comparison to Australian patients evaluated for post-surgical pain and opioid requirements after major abdominal surgeries, Chinese patients in Hong Kong were found to be associated with higher pain severity yet lower opioid consumption, which the authors attributed in part to potential differences in susceptibility to opioid-induced side effects (31) as well as the possibility that patients may appear to be more stoic and less likely to complain about pain in Chinese culture (31,33). Coupled with an increasing incidence of gynecologic cancers over time (34) as well as a booming use of surgical robotics in China (35,36), the methodological approach and implications of the study’s results may be relevant to other settings.
The findings from the current study support results from a previous study demonstrating a return to overall health-related quality of life within the three-week follow-up after robotic surgery (23). Future studies evaluating quality of life and pain following robotic surgery could consider assessing patient-reported outcomes sooner than three weeks after surgery.
Patients have ranked pain as among the worst postoperative outcomes they would hope to avoid (37,38), and the results from the current study could help alleviate some of the worry patients experience with regard to postoperative pain expectations following robotic surgery.
In conclusion, the current study shows that robotic surgery for the treatment of gynecologic cancers results in a minimal impact on patient-rated pain, little narcotic use, and positive satisfaction in the short and long term after surgery.

Full table
Acknowledgments
We would like to express our sincere gratitude to our volunteers from Hope & Cope, without whom this study would not have been possible.
Funding: This study was supported by grants from the Israel Cancer Research Fund, the Gloria’s Girls Fund, the Susan and Jonathan Wener Fund, and the Anne-Marie and Mitch Garber Fund.
Footnote
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm.2019.01.04/coif). WHG serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from Jun 2018 to May 2020. SL and WHG reports other (support for proctoring) from Minogue Medical, personal fees from Intuitive Surgical, outside the submitted work. RK reports grants from Intuitive Surgical, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Jewish General Hospital’s Research Ethics Office (protocol #09-123) and informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437-49. [Crossref] [PubMed]
- Ferrell B, Smith S, Cullinane C, et al. Symptom concerns of women with ovarian cancer. J Pain Symptom Manage 2003;25:528-38. [Crossref] [PubMed]
- Breivik H, Cherny N, Collett B, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol 2009;20:1420-33. [Crossref] [PubMed]
- van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain 2007;132:312-20. [Crossref] [PubMed]
- Pavlin DJ, Chen C, Penaloza DA, et al. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002;95:627-34. table of contents. [PubMed]
- Coley KC, Williams BA, DaPos SV, et al. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. J Clin Anesth 2002;14:349-53. [Crossref] [PubMed]
- Wells N, Murphy B, Wujcik D, et al. Pain-related distress and interference with daily life of ambulatory patients with cancer with pain. Oncol Nurs Forum 2003;30:977-86. [Crossref] [PubMed]
- Luckett T, Davidson PM, Green A, et al. Assessment and management of adult cancer pain: a systematic review and synthesis of recent qualitative studies aimed at developing insights for managing barriers and optimizing facilitators within a comprehensive framework of patient care. J Pain Symptom Manage 2013;46:229-53. [Crossref] [PubMed]
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 2006;367:1618-25. [Crossref] [PubMed]
- Voscopoulos C, Lema M. When does acute pain become chronic? Br J Anaesth 2010;105:i69-85. [Crossref] [PubMed]
- VanDenKerkhof EG, Hopman WM, Goldstein DH, et al. Impact of perioperative pain intensity, pain qualities, and opioid use on chronic pain after surgery: a prospective cohort study. Reg Anesth Pain Med 2012;37:19-27. [Crossref] [PubMed]
- Brandsborg B, Nikolajsen L, Hansen CT, et al. Risk factors for chronic pain after hysterectomy: a nationwide questionnaire and database study. Anesthesiology 2007;106:1003-12. [Crossref] [PubMed]
- Brandsborg B, Dueholm M, Nikolajsen L, et al. A prospective study of risk factors for pain persisting 4 months after hysterectomy. Clin J Pain 2009;25:263-8. [Crossref] [PubMed]
- Crombie IK, Davies HT, Macrae WA. Cut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinic. Pain 1998;76:167-71. [Crossref] [PubMed]
- Peters ML, Sommer M, de Rijke JM, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg 2007;245:487-94. [Crossref] [PubMed]
- Deandrea S, Montanari M, Moja L, et al. Prevalence of undertreatment in cancer pain. A review of published literature. Annals of Oncology 2008;19:1985-91. [Crossref] [PubMed]
- Foley KM. How well is cancer pain treated? Palliat Med 2011;25:398-401. [Crossref] [PubMed]
- Kornblith AB, Huang HQ, Walker JL, et al. Quality of Life of Patients With Endometrial Cancer Undergoing Laparoscopic International Federation of Gynecology and Obstetrics Staging Compared With Laparotomy: A Gynecologic Oncology Group Study. J Clin Oncol 2009;27:5337-42. [Crossref] [PubMed]
- Ghezzi F, Uccella S, Cromi A, et al. Postoperative pain after laparoscopic and vaginal hysterectomy for benign gynecologic disease: a randomized trial. Am J Obstet Gynecol 2010;203:118.e1-8. [Crossref] [PubMed]
- Zechmeister JR, Pua TL, Boyd LR, et al. A prospective comparison of postoperative pain and quality of life in robotic assisted vs conventional laparoscopic gynecologic surgery. Am J Obstet Gynecol 2015;212:194.e1-7. [Crossref] [PubMed]
- Leitao MM Jr, Malhotra V, Briscoe G, et al. Postoperative pain medication requirements in patients undergoing computer-assisted ("Robotic") and standard laparoscopic procedures for newly diagnosed endometrial cancer. Ann Surg Oncol 2013;20:3561-7. [Crossref] [PubMed]
- Lau S, Aubin S, Rosberger Z, et al. Health-related quality of life following robotic surgery: a pilot study. J Obstet Gynaecol Can 2014;36:1071-8. [Crossref] [PubMed]
- Abitbol J, Lau S, Ramanakumar AV, et al. Prospective quality of life outcomes following robotic surgery in gynecologic oncology. Gynecol Oncol 2014;134:144-9. [Crossref] [PubMed]
- Cleeland CS. The Brief Pain Inventory: User Guide. MD Anderson Cancer Center. 1991. Last accessed April 8, 2015. Available online: http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf
- Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994;23:129-38. [PubMed]
- Serlin RC, Mendoza TR, Nakamura Y, et al. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995;61:277-84. [Crossref] [PubMed]
- Abitbol J, Cohn R, Hunter S, et al. Minimizing pain medication use and its associated costs following robotic surgery. Gynecol Oncol 2017;144:187-92. [Crossref] [PubMed]
- Mourits MJ, Bijen CB, Arts HJ, et al. Safety of laparoscopy versus laparotomy in early-stage endometrial cancer: a randomised trial. Lancet Oncol 2010;11:763-71. [Crossref] [PubMed]
- El Hachem L, Acholonu UC Jr, Nezhat FR. Postoperative pain and recovery after conventional laparoscopy compared with robotically assisted laparoscopy. Obstet Gynecol 2013;121:547-53. [Crossref] [PubMed]
- LaVela SL, Gallan AS. Evaluation and measurement of patient experience. Patient Experience Journal 2014;1:28-36.
- Konstantatos AH, Imberger G, Angliss M, et al. A prospective cohort study comparing early opioid requirement between Chinese from Hong Kong and Caucasian Australians after major abdominal surgery. Br J Anaesth 2012;109:797-803. [Crossref] [PubMed]
- Campbell CM, Edwards RR. Ethnic differences in pain and pain management. Pain Manag 2012;2:219-30. [Crossref] [PubMed]
- Tung WC, Li Z. Pain Beliefs and Behaviors Among Chinese. Home Health Care Manag Pract 2014;27:95-7. [Crossref]
- Jiang X, Tang H, Chen T. Epidemiology of gynecologic cancers in China. J Gynecol Oncol 2018;29:e7 [Crossref] [PubMed]
- Orbis Research. Global Surgical Robots Market 2018- Segmented by Component, Area of Surgery, Region-Growth, Trends, Technology and Forecast to 2023. Thomson Reuters.
- Huan Z. Surgical robots perform over 40,000 operations in China. People’s Daily.
- Jenkins K, Grady D, Wong J, et al. Post-operative recovery: day surgery patients' preferences. Br J Anaesth 2001;86:272-4. [Crossref] [PubMed]
- Macario A, Weinger M, Carney S, et al. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg 1999;89:652-8. [PubMed]
Cite this article as: Abitbol J, Lau S, Ramanakumar AV, Drummond N, Rosberger Z, Gotlieb R, How J, Kessous R, Gotlieb WH. Evaluating postoperative pain and satisfaction among women treated by robotic surgery for gynecologic cancer. Gynecol Pelvic Med 2019;2:6.