Laparoscopic lateral suspension for apical vaginal wall prolapse: review article
Kapandji initially performed lateral suspension technique in 1967 with laparotomy access (1). Dubuisson et al. first described it in 1998 with laparoscopic approach (2). Recently, adapted by robot-assisted laparoscopy (3). Since 1998, laparoscopic lateral suspension (LLS) has gained much attention and has been performing all around the world and the technique has changed and modified over the years, as well. LLS aimed to treat apical and anterior vaginal wall prolapse.
Pelvic organ prolapse (POP) exact prevalence is not known clearly, because it is said that just about 10–20% of affected women applied to professionals (4). And lifetime risk of surgery for POP is about 12–19% (5). POP treatment is one of the challenging issues in gynecology practice due to complexity of pelvic floor anatomy, functioning and understanding. Minimal invasive surgery has gained more popularity due to certain advantages over open cases such as decreased blood loss, infection, pain and faster recovery (6).
Laparoscopic sacrocolpopexy (LSC) has admitted to be gold standard technique for the treatment of apical vaginal wall prolapse but it substantially depends on surgical skill and expertise including significant pelvic dissection. Especially, dissection at the sacral promontory sometimes tricky, particularly in obese women and patients who have anatomical variations.
LLS have comparable outcomes with regards to success, recurrence, reoperation and complication rates (7-14). In addition, LLS provides shorter operation time and requires less degree of Trendelenburg position (13). Considering apical vaginal wall prolapse is more common in elderly patient population, shorter surgery time will be an offering of LLS to this group, as well.
Operative technique
Patients are operated with general anesthesia. Patients are placed in the semi-dorsal lithotomic position.
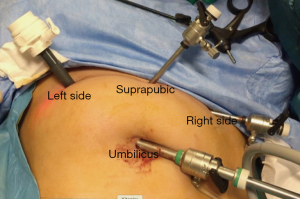
We usually utilize 4 trocars as follows; 10 mm trocar from umbilicus for 30° telescope, 10 mm trocar from left iliac area, 5-mm trocar from suprapubic area and another 5-mm trocar from right iliac area for instruments (Figure 1).
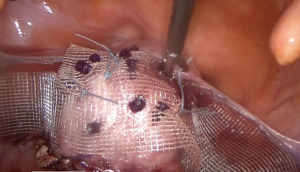
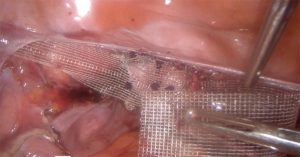
After exploration, adhesiolysis is done if needed, then bladder is dissected and freed from the vagina or cervix; dissection is carried out according to the level of cystocele. A T-shaped polypropylene mesh is prepared according to each patient. The middle part of the mesh is cut according to extent of the cystocele. Both arms of the mesh are usually about 2–3-cm wide and 20–30-cm long. Polypropylene mesh is introduced into the peritoneal cavity through the 10-mm trocar. The middle part of the mesh and its anterior part are sutured with No 0 polyester to the vagina or uterine isthmus with figure of 8 sutures, 4–6 times. Absorbable tacker or fasteners with a number of 4–6 times is another technique to fix the mesh to vagina or uterine isthmus (Figure 2). Two to 3-mm cutaneous incisions are made about 2-cm above and 4-cm lateral to the anterior superior iliac spines. Laparoscopic atraumatic forceps are entered from these incisions, perforating only the aponeurosis of the external oblique muscle to create retroperitoneal tunnels. Forceps push forward with cautiously in order to follow an avascular area with the help of laparoscope. The forceps directed to the round ligament, passed underneath till to the distal end of the mesh arm, then mesh is grasped and taken out by the help of laparoscopic forceps to the cutaneous incisions on either side (Figure 3). Now, mesh serves like a hammock to suspend the vagina or uterus, and then pulling the arm ends on either side creates desired level. The protruding ends of the mesh arms are cut below the cutaneous incision and either left unsutured or sutured to the aponeurosis of the external oblique muscles on both sides, using polyglactin 2-0 sutures at the desired level. Absorbable suture is used for reperitonealization.
Discussion
Although LSC seems to be gold standard for treating apical vaginal wall prolapse, LLS has been gaining popularity globally. LSC needs advanced level surgical skills when compared with LLS hence LSC has a steep learning curve, as well (15). Moreover, sacral promontory dissection could be difficult, especially in women who have anatomical variations and who are obese. In those women not frequently but crucial ureteral, neurological and vessel complications might be occurred.
LLS intended to treat apical and anterior vaginal wall prolapse; according to De Lancey classification uterosacral and cardinal ligaments supports the apex, cervix and proximal vagina and treatment of vault or uterine prolapse, may solve the cystocele problem as well, and in this way an unnecessary cystocele treatment can be avoided (16).
LLS technique has evolved or modified according to the surgical outcomes and innovation of technology throughout the years since first reported in 1998. Even, Dubuisson and his team have also changed the technique during this period; they started with two meshes (2,17) and changed to single mesh (8,9) also mesh types have changed from Vicryl composite meshes (mixed fiber mesh, polyglactin 910 and polyester, Ethicon) (2) or polyester meshes (8) to polypropylene meshes (Gynemesh®; Ethicon Inc., Somerville, NJ, USA) (9) or macroporous lightweight polypropylene meshes (Gynemesh®; Ethicon) or precut titanium-coated polypropylene meshes (TiLOOP®; pfm medical ag, Köln, Germany) (10-12). Varieties of non-absorbable suture and different number of sutures that fixing the meshes to the tissue have utilized, absorbable tackers or fasteners have experienced, as well. There are several modifications of LLS concerning technique itself in literature (18,19). Our group has described the Mulayim technique, that is intended to treat apical vaginal wall prolapse and which differs from original technique by utilizing Mersilene tape on a 48-mm round-bodied needle (Ethicon Inc., Somerville, NJ, USA) instead of mesh and enables easy suturing without knotting so it has the potential to be easier, shorter when compared with original described method (19).
Since 1998, literature expanding with case reports, case series, prospective trials concerning LLS. However, comparative and randomized studies are lacking with respect to anatomic, subjective outcomes and complications or side effects. Our randomized controlled trial’s preliminary result seems promising (NCT03722563).
Dubuisson and Chapron reported two cases for the first time in 1998, which they performed uterine preserving LLS and one-year after operation the results were satisfactory both anatomically and functionally (2). Later then they reported 35 cases of women with genital prolapse treated by LLS and after the mean follow-up of 10.5±4.6 months, 90.9% of the patients were satisfied with regard to the functional results (17). After then a prospective cohort study reported of which 73 patients with genital prolapse treated by LLS using a single mesh. With the regards of anatomic outcomes, 64 (87.7%) patients had successful results, POP reoccurred in 9 (12.3%) patients and 5.5% of patients had mesh erosion following for a median of 19 [12–41] months (8). Dubuisson et al. this time, prospectively studied patients who had vault prolapse, treated with LLS with respect to the long-term outcomes. After surgery, following a mean of 17.5 months, recurrent vaginal vault prolapse was occurred just in one woman, with a success of 98.6%. Four patients reported presenting with mesh erosion into the vagina among 73 patients. Also, they mentioned that LLS is primarily for apical and anterior vaginal wall prolapse treatment, not for evident rectocele repair and added that performing a posterior colporrhaphy vaginally in the regard of evident rectocele could prevent recurrent prolapse because there were no recurrences occurred when they performed posterior colporrhaphy (9). So, in our opinion, concomitant posterior patch attaching to rectovaginal space laparoscopically or posterior colporrhaphy vaginally would be supposed to be done during LLS in the regard of evident rectocele, as well.
Veit-Rubin et al. reported of 245 patients who had POP treated with LLS while saving uterus. Following 1-year, success rates were 88.2%, 86.1% and 80.8% for anterior, apical and posterior compartments, respectively. Mesh exposure was occurred in three patients (1.2%) in women preserving uterus that was less than aforementioned above studies. Same group also mentioned that while performing LSC, sacral promontory dissection could be difficult, especially in women who had anatomical variations and who were obese. LLS could prevent some of rare but crucial complications such as neurological or ureteral and vessel injury that might be occurred during LSC (10).
Later on, Veit-Rubin et al. showed that saving the uterus did lead better outcomes both anatomically and subjectively when performing LLS compared with LLS with hysterectomy patients among 339 women who had symptomatic cystocele and/or uterine prolapse. Because performing hysterectomy alone does not address the deficiencies in pelvic support and does not correct the underlying pathophysiology, so in the absence of uterine disease, uterus should be preserved. Hence, LLS operation concomitant with hysterectomy or not, is a safe method with high patient satisfaction (11).
Veit-Rubin et al. reported satisfaction of 417 patients after treated with LLS who had POP. Following 1 year after surgery, 78.4% of patients had no symptoms and anatomic success rates were; 91.6%, 93.6% and 85.3% for the anterior, apical and posterior compartments, respectively. With respect to Clavien-Dindo classification, 2.2% of patients had grade III or higher complications. The mesh complication rate was 4.3%. Two hundred and fourteen patients could be reached with telephone interview among 417 patients, following a mean of 7.2 years after surgery and over 85% rated their situation as improved (12).
Dällenbach et al. reported that the risk of mesh erosion after LLS operation was 3.8%, following after a mean of 82.3 months (range, 28.2–130.6 months). They found that there were two important risk factors; tobacco use and mesh type. Type 1 mesh; macroporous, monofilamentous polypropylene mesh should be preferred against multifilamentous or microporous type 3 mesh and they concluded that risk of mesh erosion was low and could be more diminished by utilizing the proper mesh material, and by paying attention to the patient characteristics like smoking (20).
A retrospective study from Martinello et al. showed that success of POP treatment with LLS after 12 months of surgery was 92% and 100% for anterior and apical compartments, respectively. No de novo, evident rectoceles was reported and concerning de novo urinary incontinence, total of three patients were reported during one year after surgery. The complications reported with respect to Clavien-Dindo classification were as follows, one patient for grade 2 and three patients for grade 3. There were no mesh complications. The mean duration of LLS operation was 104 min that was far shorter when compared to LSC, 199±46 min (13).
A prospective double center study from Italy which evaluated the treatment of apical and anterior vaginal wall prolapse with LLS according to long-term outcomes and complications showed that at 2 years 89% of patients were asymptomatic and anatomic success rate was 94.2% and 94.9% for the anterior and apical compartments, respectively. And unlike doubts concerning LLS treatment for apical and anterior vaginal wall prolapse; results suggested that LLS did not lead to enterocele or hernia at the posterior cul-de-sac. Only one mesh erosion occurred among 120 patients, which was 1 month after surgery that a titanium-coated macroporous polypropylene mesh (TiLOOP® Dubuisson) was used as for all patients, too. This is much less than previous reported incidences. This is may be because of what Dällenbach et al. mentioned about mesh types. Thirteen patients had various urogynecological de novo symptoms such as urgency, stress urinary incontinence and transient voiding obstruction. De novo constipation, fecal incontinence or dyspareunia was not reported. In their cohort of patients who underwent LLS, postoperative Clavien-Dindo grade 3 or more complications occurred only in 1/119 of cases (14).
Hence, LLS treatment for apical vaginal wall prolapse should not be concerned only when avoiding dissection at the sacral promontory as back up procedure because LLS treatment for apical and anterior vaginal wall prolapse is successful with regard to anatomic and subjective outcomes and can be performed by all gynecologic laparoscopist with safety because it does not depend much expertise. However, prospective studies and prospective randomized controlled trials concerning LLS are lacking, comparing with other treatments with respect to apical vaginal wall prolapse.
Acknowledgments
I would like to thank to guest editor Dr. Gokhan Sami Kılıc for kind invitation and support.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Gokhan Kilic) for the series “Minimally Invasive Treatment Modalities for Female Pelvic Floor Disorders” published in Gynecology and Pelvic Medicine. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-2020-pfd-02/coif). The series “Minimally Invasive Treatment Modalities for Female Pelvic Floor Disorders” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kapandji M. Cure des prolapsus uro-génitaux par colpo-isthmo-cystopexie par bandelettes transversales et la douglassoraphie ligamentopéritonéale étagée et croisée. Ann Chir 1967;21:321-8. [PubMed]
- Dubuisson JB, Chapron C. Laparoscopic iliac colpo-uterine suspension for treatment of genital prolapse using two meshes. A new operative technique. J Gynecol Surg 1998;14:153-9. [Crossref]
- Simoncini T, Russo E, Mannella P, et al. Robotic-assisted apical lateral suspension for advanced pelvic organ prolapse: surgical technique and perioperative outcomes. Surg Endosc 2016;30:5647-55. [Crossref] [PubMed]
- Barber MD, Maher C. Apical prolapse. Int Urogynecol J 2013;24:1815-33. [Crossref] [PubMed]
- Smith FJ, Holman CD, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organprolapse. Obstet Gynecol 2010;116:1096-100. [Crossref] [PubMed]
- Agha R, Muir G. Does laparoscopic surgery spell the end of the open surgeon? J R Soc Med 2003;96:544-6. [Crossref] [PubMed]
- Szymczak P, Grzybowska ME, Wydra DG. Comparison of laparoscopic techniques for apical organ prolapse repair - a systematic review of the literature. Neurourol Urodyn 2019;38:2031-50. [Crossref] [PubMed]
- Dubuisson JB, Yaron M, Wenger JM, et al. Treatment of genital prolapse by laparoscopic lateral suspension using mesh: a series of 73 patients. J Minim Invasive Gynecol 2008;15:49-55. [Crossref] [PubMed]
- Dubuisson J, Eperon I, Dällenbach P, et al. Laparoscopic repair of vaginal vault prolapse by lateral suspensionwith mesh. Arch Gynecol Obstet 2013;287:307-12. [Crossref] [PubMed]
- Veit-Rubin N, Dubuisson JB, Lange S, et al. Uterus-preserving laparoscopic lateral suspension with mesh for pelvic organ prolapse: a patient-centred outcome report and video of a continuous series of 245 patients. Int Urogynecol J 2016;27:491-3. [Crossref] [PubMed]
- Veit-Rubin N, Dubuisson J, Constantin F, et al. Uterus preservation is superior to hysterectomy when performing laparoscopic lateral suspension with mesh. Int Urogynecol J 2019;30:557-64. [Crossref] [PubMed]
- Veit-Rubin N, Dubuisson JB, Gayet-Ageron A, et al. Patient satisfaction after laparoscopic lateral suspension with mesh for pelvic organ prolapse: outcome report of a continuous series of 417 patients. Int Urogynecol J 2017;28:1685-93. [Crossref] [PubMed]
- Martinello R, Scutiero G, Stuto A, et al. Correction of pelvic organ prolapse by laparoscopic lateral suspension with mesh: A clinical series. Eur J Obstet Gynecol Reprod Biol 2019;240:351-6. [Crossref] [PubMed]
- Mereu L, Tateo S, D'Alterio MN, et al. Laparoscopic lateral suspension with mesh for apical and anterior pelvic organ prolapse: A prospective double center study. Eur J Obstet Gynecol Reprod Biol 2020;244:16-20. [Crossref] [PubMed]
- Claerhout F, De Ridder D, Roovers JP, et al. Medium-term anatomic and functional results of laparoscopic sacrocolpopexy beyond the learning curve. Eur Urol 2009;55:1459-67. [Crossref] [PubMed]
- Rahmanou P, White B, Price N, et al. Laparoscopic hysteropexy: 1- to 4-year follow-up of women postoperatively. Int Urogynecol J 2014;25:131-8. [Crossref] [PubMed]
- Dubuisson JB, Chapron C, Fauconnier A, et al. Laparoscopic management of genital prolapse: lateral suspension with two meshes. Gynaecol Endosc 2000;9:3683-9. [Crossref]
- Mereu L, Dalpra F, Terreno E, et al. Mini-Laparoscopic Repair of Apical Pelvic Organ Prolapse (POP) by Lateral Suspension with Mesh. Facts Views Vis Obgyn 2018;10:139-45. [PubMed]
- Mulayim B, Sendag F. Modified Laparoscopic Lateral Suspension: The Mulayim Technique. J Minim Invasive Gynecol 2019;26:407-8. [Crossref] [PubMed]
- Dällenbach P, De Oliveira SS, Marras S, et al. Incidence and risk factors for mesh erosion after laparoscopic repair of pelvic organ prolapse by lateral suspension with mesh. Int Urogynecol J 2016;27:1347-55. [Crossref] [PubMed]
Cite this article as: Mulayim B. Laparoscopic lateral suspension for apical vaginal wall prolapse: review article. Gynecol Pelvic Med 2020;3:22.