The unusual case of vaginal calculus in an eighty-four-year-old woman: a case report
Highlight box
Key findings
• Vaginal calculus, primary and secondary.
What is known and what is new?
• Vaginal calculi are a rare finding and are typically primary in nature without a nidus usually due to urinary stasis.
• This case report describes a secondary calculus due to a nidus from a previous vaginal surgery and the full evaluation and management of the vaginal stone.
What is the implication, and what should change now?
• The rarity of this case adds to the literature concerning the formation, understanding the pathophysiology and the treatment of vaginal stones.
Introduction
Vaginal calculi, also referred to in the literature as colpolithiasis or vaginal stones, are a rare gynecologic finding. The first vaginal calculi were described as early as 1900 (1), and have been elaborated on since that time only as case reports or meta-analyses of separate case reports, given their rarity. They occur in a variety of ages from toddlers to adults with a range of presentations (2), and their detection warrants reporting in the medical journals. This case is especially unique because the patient is the oldest reported in the literature at 84 years.
Characteristically, vaginal stones are uroliths. Uroliths form because of mineral deposition, usually due to urinary stasis or a material that incites mineral aggregation. Colpolithiasis occur secondary to other medical comorbidities, most notably urogenital malformations and fistulas (2). Whether or not they are symptomatic, they can act as a nidus for infection and thus vaginal stones are often removed either surgically or with lithotripsy according to provider judgment and patient preference (2,3). If the underlying cause of the stone can be corrected, patients reportedly experience remission of their presenting symptoms, though little data on long term follow up exist (4,5). We present this case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-17/rc).
Case presentation
An 84-year-old gravida 5 para 5 presented to a private gynecologist in Summersville, West Virginia, USA, for a “hard knot” in the vagina. She first noticed the mass when wiping two years prior to the visit and it has since grown larger. She denied pain, dysuria, urinary obstruction, and urinary pooling, but found the mass uncomfortable. She was not sexually active. The patient last saw a gynecologist 20 years prior for an anterior colporrhaphy for pelvic organ prolapse with recurrent stress urinary incontinence. Gynecologic history was significant for stress urinary incontinence and a vaginal hysterectomy approximately 40 years prior to her visit. Her five pregnancies were all term, spontaneous vaginal deliveries. Figure 1 demonstrates a simple timeline of her past medical history. She had a history of normal pap smears throughout her life. She denied any other gynecologic complaints, including bleeding, discharge, pelvic pain, or gastrointestinal symptoms. Medical history was notable for carotid stenosis, hyperlipidemia, history of stroke, hypertension, major depression, and mild dementia.
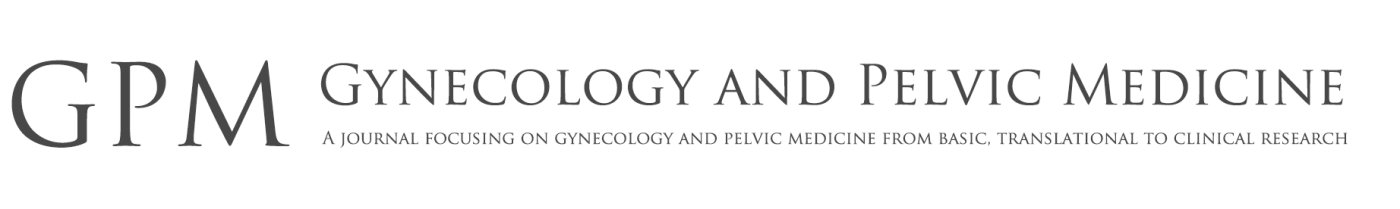
Upon physical exam, her vulva and vaginal epithelium were expectedly atrophic. Her urethral meatus was not obstructed. After separating the labia there appeared to be a vaginal stone approximately 1 cm cephalad to the hymenal ring. Patient discomfort secondary to atrophy and mild agglutination limited the in-office assessment of the size and extent of the stone. The patient was consented for an exam under anesthesia with removal of the vaginal mass.
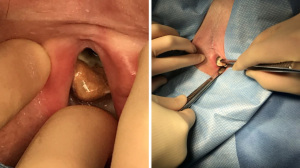
After obtaining the proper medical clearance and consenting to the procedure, she was placed under conscious sedation. After a thorough exam, 1 cm cephalad to the hymenal ring along the posterior vaginal epithelium was a 2.5 cm × 2.0 cm × 1.2 cm stone (see Figures 2,3). The colpolith was wall demarcated with a limited attachment to the posterior vaginal wall. A rectal exam was done demonstrating no rectal involvement. During the exam, the patient coughed and leaked urine, confirming stress urinary incontinence. There was no evidence of fistulous tract in the vagina. Other than expected atrophy, the vagina was unremarkable. Given the findings of the exam under anesthesia, no further imaging or diagnostic modalities were felt to be necessary in this case. Local anesthesia was applied to the peripheral region around the stone. Using a number 15 blade and curved mayo scissors, the vaginal stone was excised, measured, and sent to pathology for further analysis. Gross observation showed a minimally granular dull, dark yellowy brown calculus with a depressed, dark brown focus on one side that contained a 1.2 cm × 0.9 cm × 0.5 cm tan-pink, rubbery tissue with bright blue synthetic suture incorporated into the soft tissue. She recovered without complication and went home the same day of surgery with xylocaine jelly and Premarin cream for postoperative pain and tissue healing, respectively.
Pathologic report from our institution noted this as a calculus mass consistent with a urolith with suture material noted in the peripheral soft tissue removed during dissection. Additionally, a focus of suture was found on the innermost aspect of the calculus, with approximately 1.5 cm of permanent suture discovered. The specimen was sent to Mayo Clinic for a second opinion. Mayo reported the calculus as 80% struvite, 20% apatite. The patient recovered well and did not have any postoperative issues.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Vaginal calculus is a rare diagnosis and occurs over an extended course of time. Risk factors include urogenital anomalies, obstructive vaginopathies, severe neurological disease, bed-bound status, vaginal infections, hypoestrogenic state, and incontinence. The pathology revolves around pooling of urine in the vagina, which in turn allows for urogenic calculus formation. Vaginal infections and lack of estrogen cause changes in vaginal flora and lead to an increase in pH. This change in acidity increases the likelihood of stone formation (2,3).
Generally, vaginal calculi are categorized as either primary or secondary. Traditionally, primary calculi are considered more common and represent most vaginal stone case reports, though true incidence has never been elucidated given their rarity (6,7). Primary vaginal stones are a calculus aggregation without nidus, usually in the setting of urinary stasis; many patients are bedridden, have a neurologic condition causing incontinence, or anatomic abnormality allowing urine to pool (2). Infrequently, blood acts as an aggregating medium, particularly in individuals with vaginal obstructive disorders (2). The most common coexisting condition is vesicovaginal fistula, which has been well-described in the literature as a strong predisposing risk factor (8).
Secondary vaginal stones occur when there is a nadir of aggregation. Besides the presence of a foreign entity, the preexisting risk factors for occurrence are identical to primary stones. Case reports have included mesh (8), suture (6), intrauterine devices (IUDs) (4), household foreign bodies (9), and pessaries (7) as foci for secondary stones to develop, which may be iatrogenic. It is not unusual for patients with a secondary vaginal stone to also have a vesicovaginal fistula (5).
Diagnosis is critical and a thorough history and physical should be utilized. Examination alone classically is sufficient for confirmation, but imaging studies such as X-ray or ultrasound have been used to assist in diagnosis (3,9). These provide a clear image of the stone’s presence and may be useful in patients who cannot tolerate an exam. On occasion, computed tomography (CT) and magnetic resonance imaging (MRI) may be used with great accuracy in pinpointing the calculus (9,10). However, these modalities are more expensive and time consuming and are rarely needed.
The treatment for primary and secondary colpolithiasis is the same: exam under anesthesia with removal of the stone. The methodology may range from lithotripsy to stone dismantling to local debridement of involved tissue (3). Stones may vary in their size, although usually they are 4–5 cm in diameter (2). Resection and therein repair may be extensive, depending on the involvement of the stone into the vaginal epithelium and size of stone. Any obvious inciting pathology, such as suture material, are to be removed (2). Often, topical estrogens may be considered to facilitate tissue healing, especially in a hypoestrogenic state (7). Calculi are typically sent to pathology thereafter for mineral analysis and to investigate a possible nidus. Pathology may reveal a number of mineral combinations, but struvite (ammonium-magnesium phosphate) is the most common and usually is the major component. If a fistulous process is present, delayed repair of the fistula approximately three to six months from stone removal has been suggested (3).
Our patient was found to have a secondary vaginal calculus, given the presence of suture material deep within the stone. Initially, the authors pre- and intraoperatively suspected a primary stone based on her stress urinary incontinence and lack of surgical history involving the posterior vagina, where the stone was located; thus, the discovery of suture material came as a surprise. Unlike primary stones, older patients are more commonly affected by secondary vaginal stones (1), perhaps because this demographic typically are hypoestrogenic and may have stress urinary incontinence (7,8). Our patient had these comorbidities and will be the oldest patient with a vaginal stone reported in the literature.
This presentation was especially unique because our patient did not have a vesicovaginal fistula. A thorough exam under anesthesia, patient history, and physical did not reveal any evidence of fistulous conditions nor other vaginal obstructive disease such as agglutination or septations. Additionally, our patient was very active and did not have any deconditioning risk factors. The general pathophysiology typically revolves around urinary pooling within the vagina, which would be unusual in a woman without a fistula, vaginal obstruction, or limited mobility.
Conclusions
The case described is one of very few reported vaginal calculi and therefore we experienced several limitations. As is the case with any rare case report, it is not feasible to extrapolate our approach or findings to conclusive clinical care for others with the same diagnosis. Therefore, it would be difficult to design future studies to be adequately powered. As well, this patient was new to our practice and previously had not had consistent gynecologic care for the better part of the last two decades. This well pre-dates most electronic medical records and without definitive access to past records due to her former physician retiring, it is difficult to fully describe her disease course. This is most notable with her past surgical history, given the suture material found in the vaginal stone. Having full access to her medical records and operative reports would have provided valuable insight into the pathological process and thus a wealthy source of information.
The strength of the case report is in the rarity of the case and comprehensive diagnosis and management of the stone. Additions to the literature when rare cases are encountered are incredibly important to not only understanding a rare condition, but as well as to unfold different aspects of pathophysiology and to further understanding our discipline.
Acknowledgments
We would like to extend our greatest thanks to this patient for trusting her care with us and allowing us to share her story with the greater medical community to deepen understanding of rare presentations and conditions.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-17/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-17/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-17/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Navani S, Tessier PA. A primary vaginal stone. Br J Radiol 1970;43:222-3. [Crossref] [PubMed]
- Jo JY, Lee SM, Shin JK, et al. Huge vaginal stone: Case report and review of the literature. Front Surg 2022;9:937371. [Crossref] [PubMed]
- Wei D, Xie Y, Niu X. Vaginal stones caused by urethrovaginal fistula: A case report. Medicine (Baltimore) 2019;98:e18003. [Crossref] [PubMed]
- Beedham T, Rao K. Giant vaginal stone with embedded contraceptive device. J R Soc Med 2001;94:522-3. [Crossref] [PubMed]
- Kurmanov TA, Kulkayeva GU, Shakirova AF, et al. Primary vaginal stone associated with vesicovaginal fistula: A case report. Urol Case Rep 2022;40:101917. [Crossref] [PubMed]
- Tavakkoli M, Ghoreifi A. Large vaginal and bladder calculi in a woman with previous operation of bladder exstrophy: a case report. Nephrourol Mon 2014;6:e13637. [PubMed]
- Shailaja C, Dhurba U, Shanti S, et al. Secondary Vaginal Stone Around a Forgotten Vaginal Pessary in a Patient with a Vesicovaginal Fistula. South Asian Federation of Obstetrics and Gynecology 2009;1:53-4. [Crossref]
- Griffiths KM, Towers GD, Yaklic JL. Vaginal Urinary Calculi Formation Secondary to Vaginal Mesh Exposure with Urinary Incontinence. Case Rep Obstet Gynecol 2017;2017:8710315. [Crossref] [PubMed]
- Surya M, Sharma C, Sood D, et al. Neglected vaginal foreign body leading to vaginolith, vesicovaginal fistula and vesical calculus formation in an adolescent girl. BJR Case Rep 2016;2:20150474. [Crossref] [PubMed]
- Zilberlicht A, Feiner B, Haya N, et al. Surgical removal of a large vaginal calculus formed after a tension-free vaginal tape procedure. Int Urogynecol J 2016;27:1771-2. [Crossref] [PubMed]
Cite this article as: Corcoran CJ, Williams E, Bush SH. The unusual case of vaginal calculus in an eighty-four-year-old woman: a case report. Gynecol Pelvic Med 2023;6:17.