Patient counseling for pelvic organ prolapse surgery: methods used for patient education
Highlight box
Key findings
• Personal interviews is the most common primary in-office method of patient education and distributing standardized print materials is the most common supplementary method.
• Simple language and providing print materials are the most utilized communication techniques in pelvic organ prolapse (POP) counseling.
• Many important complications of POP procedures are not discussed in detail.
What is known and what is new?
• POP is a complex condition and patients undergoing surgery for POP are often inadequately informed about their condition and procedure.
• Our survey is the first to characterize the practice patterns of a sample of Female Pelvic Medicine and Reconstructive Surgery providers.
What is the implication, and what should change now?
• Evidence-based approaches for patient education for POP should be developed and implemented.
• Future investigations should evaluate educational preferences from the patient perspective.
Introduction
Pelvic organ prolapse (POP) is a pelvic floor disorder that occurs in up to 50% of women (1). POP can result in bothersome symptoms, including pelvic pressure, pelvic pain, a sensation of bulge, and back pain. Approximately 13% of women undergo POP surgery to alleviate these symptoms (2,3). Symptoms associated with POP are often complex, may overlap with other pelvic floor disorders, and may not be alleviated with prolapse surgery alone. Therefore, comprehensive counseling with expectation management is essential for women planning to undergo POP surgery.
Preoperative patient education is a crucial element of the surgical experience. Studies have shown that preoperative information and psychological preparation can enhance postoperative outcomes through improvements in postoperative pain, behavioral recovery, and even shorter postoperative hospital stay length (4,5). In other surgical subspecialties, implementation of a preoperative education program was shown to be associated with an almost 30% reduction in postoperative length of stay (6). In women undergoing pelvic reconstructive surgery, preparedness is associated with satisfaction, symptomatic improvement, and improved quality of life (7). Despite the benefit of preoperative counseling, multiple studies show that patients undergoing surgery for POP are often inadequately informed about their condition and procedure (8,9). Furthermore, due to the complexity of POP, it has been found that even patients with high health literacy, defined as patients who can readily obtain, read, and understand healthcare information (10), have difficulty understanding complex conditions such as POP (11).
To better understand the quality of preoperative counseling, we conducted a pilot study where we surveyed providers that counsel women with POP on their practice patterns. Our primary objective was to characterize the methods used, patient education materials (PEMs) offered, and content discussed by providers during preoperative counseling. Our secondary objective was to determine what communication techniques were being used to counsel patients. Our aim was to gather information on practice patterns and drive future hypotheses to determine potential areas of improvement in POP education. We present this article in accordance with the SURGE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-16/rc).
Methods
Modified from prior practice pattern surveys (12,13), we created an anonymous survey containing 73 items to assess current practices in preoperative patient counseling for POP surgery (Appendix 1). The content of our questionnaire was created by experts in POP and health literacy. Attending physicians, trainees, physician assistants, nurse practitioners, and nurses who treat POP were invited to participate in this pilot study. The survey queried providers about four major themes: demographics of their practice, patient education methods and PEMs, topics discussed during counseling, and communication techniques. The survey inquired whether complications were discussed in detail, mentioned, or not discussed in the preoperative counseling. Providers were asked to estimate the average health literacy of their patient population from very poor to excellent.
A survey link was distributed by snowball sampling via e-mail, Twitter, and Facebook groups for Female Pelvic Medicine and Reconstructive Surgery (FPMRS) providers between May–September 2019. In the first phase in May 2019, the survey was emailed to a list of FPMRS providers to calculate a response rate for the survey. Providers were requested to take the survey only once. Data collection ended in September 2019. Providers who counseled less than six patients per year (one every other month) were excluded. The survey was created, and data was managed on REDCap. Descriptive analysis was conducted via Stata/SE 14.2 (College Station, TX, USA). Means and standard deviations (SD) were computed for continuous variables.
Results
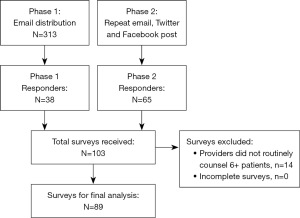
We received a total of 103 responses. Our response rate was about 12%. Fourteen participants were excluded because they did not annually counsel at least six patients for a total of 89 surveys included in the final analysis (Figure 1).
The majority of respondents were attending physicians (n=77), followed by physician assistants (n=6), trainees (n=5), and one nurse practitioner (Table 1). Approximately two-thirds of respondents were female. Provider age ranged from 29 to 67 with a mean and SD of 44±9 years. Half of the providers (51%) were less than 10 years out from training, and the majority worked in either urban teaching hospitals (64%) or private group practices (22%). Respondents reported counseling anywhere from 7 to 600 patients undergoing POP surgery per year with a mean of 100±101. Most providers (78%) reported their patient population to have a mix of government or commercial insurance and estimated the health literacy of their patient populations as either fair (43%) or good (42%). Respondents spent an average of 31±19 minutes counseling their patients. Counseling times ranged from 10 to 120 minutes, with an interquartile range of 20–40 minutes.
Table 1
| Characteristic | Value |
|---|---|
| Provider type | |
| Attending physician | 77 [87] |
| Physician assistant | 6 [7] |
| Nurse practitioner | 1 [1] |
| Trainee (resident or fellow) | 5 [6] |
| Provider gender | |
| Female | 58 [65] |
| Male | 29 [33] |
| Prefer not to say | 2 [2] |
| Age of provider (year) | 44±9 |
| 20–29 | 1 [1] |
| 30–39 | 30 [34] |
| 40–49 | 37 [42] |
| 50–59 | 17 [19] |
| 60–69 | 4 [4] |
| Years of practice after training | |
| 0–4 | 29 [33] |
| 5–9 | 16 [18] |
| 10–14 | 19 [21] |
| 15–19 | 14 [16] |
| 20+ | 11 [12] |
| Practice setting | |
| Urban teaching hospital | 57 [64] |
| Group private practice | 20 [22] |
| Urban non-teaching hospital | 4 [4] |
| Rural hospital | 4 [4] |
| Other | 4 [4] |
| Patients counseled/year | 100±101; 60 [25–120] |
| 1st quartile | 7–30 |
| 2nd quartile | 31–60 |
| 3rd quartile | 61–130 |
| 4th quartile | 131–600 |
| Payer mix | |
| Fairly even between commercial & government payers | 69 [78] |
| Mostly commercial payers | 3 [3] |
| Mix of cash and other payers | 1 [1] |
| Mostly government payers | 16 [18] |
| Health literacy of patient population | |
| Very poor | 4 [4] |
| Poor | 4 [4] |
| Fair | 38 [43] |
| Good | 37 [42] |
| Excellent | 5 [6] |
| Time spent counseling (minutes) | 31±19; 30 [20–40] |
Data are presented as n [%], mean ± SD, or median [IQR]. POP, pelvic organ prolapse; SD, standard deviation; IQR, interquartile range.
The most common primary in-office method of patient education was through personal interviews (78%) or speaking directly to the patient (Table 2). Other reported primary methods included the use of drawn or printed illustrations (n=10), using print materials such as brochures (n=9). One provider used models or props. Standardized print materials, drawn or printed illustrations, models or props, and websites were commonly used supplemental methods. The International Urogynecological Association (IUGA) was the most common source for print materials (30 of 62, 48%) used by half the providers that utilized print materials. The Society of Urodynamics, Female Pelvic Medicine, and Urogenital Reconstruction (SUFU) (37%) and American Urogynecologic Society (AUGS) (31%) were other popular sources. For those who referred patients to a website (n=13), AUGS (69%) and SUFU (54%) were the most common referred websites. Few providers used instructional videos (n=4) or smartphone applications (n=3); however, when used, YouTube and the AUGS POPQ Interactive Assessment Tool were the most popular, respectively.
Table 2
| Method/material | N [%] |
|---|---|
| Primary in-office method | |
| Personal interview | 69 [78] |
| Drawn/printed illustration | 10 [11] |
| Print material (brochures) | 9 [10] |
| Models/props | 1 [1] |
| Additional methods | |
| Standardized print material | 62 [70] |
| Drawn or printed illustrations | 51 [57] |
| Models or props | 34 [38] |
| Websites | 13 [15] |
| Instructional videos | 4 [4] |
| Smartphone or tablet applications | 3 [3] |
| Sources of print material | |
| IUGA | 30 [34] |
| SUFU | 23 [26] |
| AUGS | 19 [21] |
| ICS | 19 [21] |
| Urology Care Foundation | 8 [9] |
| UpToDate® | 2 [2] |
| Own materials | 28 [31] |
| Other (majority reported industry material) | 10 [11] |
| Websites | |
| AUGS | 9 [10] |
| SUFU | 7 [8] |
| Urology Care Foundation | 3 [3] |
| ICS | 2 [2] |
| IUGA | 1 [1] |
| Medical online information services (i.e., MedlinePlus®, WebMD, etc.) | 1 [1] |
| Other | 2 [2] |
| Sources of video material | |
| YouTube | 3 [3] |
| Own materials | 1 [1] |
| Applications | |
| AUGS POP Q Interactive Assessment Tool | 2 [2] |
| Topics included when counseling patients about POP | |
| Anatomy of POP | 89 [100] |
| Observation as a treatment | 89 [100] |
| Use of native tissues | 89 [100] |
| Surgical approach | 88 [99] |
| Causes of POP | 87 [98] |
| Postoperative hospital course | 87 [98] |
| Pessary as treatment | 85 [96] |
| Management of uterus (if applicable) | 85 [96] |
| Use of Foley catheter postoperatively | 85 [96] |
| Patients’ own role in postoperative recovery | 85 [96] |
| Use of mesh | 78 [88] |
| Pelvic floor physical therapy as a treatment | 75 [84] |
| Postoperative use of analgesia | 73 [82] |
| Use of biologics | 41 [46] |
IUGA, International Urogynecological Association; SUFU, Society of Urodynamics, Female Pelvic Medicine, and Urogenital Reconstruction; AUGS, American Urogynecologic Society; ICS, International Continence Society; POP, pelvic organ prolapse.
All providers reported that they counseled women on the anatomy of POP, observation as a treatment option, and the use of native tissues during surgery. The majority of providers discussed various surgical approaches (99%), causes of POP (98%), the postoperative hospital course (98%), pessary as a treatment (96%), management of the uterus when applicable (96%), use of a Foley catheter postoperatively (96%), and the patients’ role in recovery after surgery (96%). Fewer providers reported including the use of mesh (88%), pelvic floor physical therapy as a treatment option (84%), and postoperative use of analgesia (82%). Less than half (46%) discussed the use of biologics in surgery.
Mesh complications, when applicable (68%), urinary incontinence (66%), and the need for repeat surgery (52%) were discussed in detail by most providers. Urinary retention, injury to surrounding structures, storage lower urinary tract symptoms, dyspareunia, bleeding, infection, and constipation were more often mentioned rather than discussed. A substantial number of providers neither discussed nor mentioned constipation (17%) or dyspareunia (12%) as potential complications (Figure 2A).
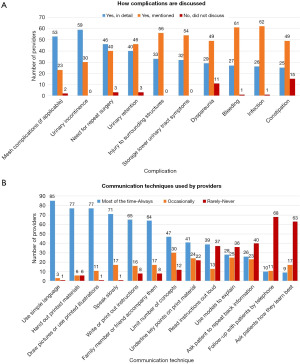
When asked about communication techniques for counseling, most providers reported using simple language (95%), giving their patients printed materials (87%), using illustrations (87%), and speaking slowly (80%) most or all the time (Figure 2B). Very few providers routinely followed up with patients by telephone (11%) or asked how they learned best (10%). Ten respondents (11%) stated that they asked patients to provide evaluation or feedback for the counseling they received.
Discussion
There is growing evidence to support that women are inadequately informed prior to urogynecological procedures (8,9,11). As a result, women fail to receive the many proven benefits of proper preoperative surgical education. Our study sought to characterize healthcare practitioners’ current practice patterns when counseling their patients on POP surgery. Our data revealed that a personal interview, where the provider engages in a dialogue with the patient, was the most common method of delivering preoperative patient education. Many providers reported supplementing a personal interview with instructions, illustrations, models, and references to websites or other materials. This is something that patients with POP desire, but do not always receive (14). Evidence suggests that written information as an adjunct to professional consultation can improve knowledge and recall (15). Fewer providers in our study opted to use educational videos, but this educational modality may be helpful as well. Patient-based educational videos developed for procedures ranging from sacral nerve stimulation to lung surgery were associated with improved patient knowledge and patient preparedness (16,17). Certain modalities and methods may be better than others. A study comparing an iPad application to standard verbal counseling found the application did not improve comprehension and was associated with worse information retention (18). The reasons why providers use specific patient education techniques are likely multifactorial. Familiarity and comfort with certain techniques may determine provider counseling preferences. Also, offering certain PEMs such as video links to watch at home may be viewed as less helpful based on preconceived notions that patients will not take the time to watch the video or lack of insight on which available videos are most accurate and understandable. This, however, would be a good area to focus some time on as patients are motivated to learn on their own and look to their providers to provide them with quality resources (14).
Our survey found that providers seem to be thorough in explaining the condition of POP, the treatment options, and what can be expected after surgery. However, many providers only mention rather than discuss common complications in detail such as injury to surrounding structures and storage lower urinary tract symptoms. They do not mention complications such as dyspareunia at all. This is consistent with prior research that identified many providers believe that explaining the treatment and stating a list of complications is sufficient counseling (19). It has been demonstrated that nearly a third of patients counseled on sacrocolpopexy in preoperative visits believed there is no risk of recurrent prolapse after surgery on subsequent knowledge assessment immediately before their procedure (8). Based on our study results, this finding is not inconceivable. While most of our respondents mentioned the “need for repeat surgery” as a complication in their counseling, only half stated they described what that meant in detail. With studies showing that patients forget up to 80% of the information given by their healthcare practitioners (20), providers should make an effort to utilize strategies and communication techniques that improve patients’ recall.
Our respondents did report using a variety of communication techniques to convey their counseling. Virtually all providers used simple language as a strategy. Our respondents described their patients as having fair or good health literacy; however, providers tend to overestimate the health literacy of their patients (21). Strategies that have been shown to improve patient verbal comprehension of the informed consent include discussion with test/feedback or repeat-back and interactive digital interventions (22). The repeat-back strategy was one of the less popular techniques in our study, used by about 30% of providers.
Other strategies for improved communication that were popular amongst respondents included “hand out printed material” and “write or print out instructions”. Readability must be taken into consideration when distributing these types of resources. Based on literacy rates of the United States, the National Institutes of Health recommends that health materials be written at the sixth to seventh-grade level (23). Students in these grades are typically 11–13 years old. The grade level of PEMs from professional urologic and urogynecologic societies for POP materials has been estimated on average to be a twelfth-grade level (24), the last year of secondary school when students are about 18 years old. Therefore, it is important that providers assess the reading grade level of PEMs prior to administering them to patients to ensure they are appropriate for the average patient. Providers can assess the grade level of their materials by using the Readability function in Word proofing options, or one of many online tools that can test readability. Patients who do not speak the native language of the country they live in are also frequently seen in practice and must be considered. Communication can be improved with these patients by having access to reliable and accurate translation services and PEMs written in multiple languages in the office.
Patient education is not a one-size-fits-all approach. Certain techniques may work for some and not others, and patients are the best source on how they learn well or whether the counseling they received made sense to them. Only 11% of respondents reported requesting patient feedback on their counseling using after-visit surveys and questions. Providers should be asking for feedback more frequently and ask for it appropriately by avoiding yes/no questions like “do you have any more questions?”. Instead, ask for feedback with “what questions do you have?”.
Of course, patient education and implementation of these strategies take up valuable time, a limited resource for many providers. Our respondents spent an average of half an hour counseling patients. With the lack of qualitative analysis of actual counseling content in our survey, it is difficult to assess if this is sufficient. And, due to limitations of clinical practice, it may be challenging to spend more than 30 minutes with patients per visit. Studies have shown that implementing interventions such as teach-back may take as few as 2–3 additional minutes while improving patient comprehension compared to standard informed consent (22). Therefore, implementing these methods may be time-saving. We also can not underestimate the time it takes to learn these techniques. Health literacy and counseling patients are not heavily emphasized in most medical school curricula or residency programs. However, student-provided patient education can improve both quality of care and medical education (25). Implementing this curriculum early in medical education will help more seamlessly incorporate these techniques into clinical practice.
Our study was not without limitations. Firstly, we were unable to evaluate the construct validity or reliability of our survey. Due to the anonymous nature of our study, we could not ascertain that responders were actually our target population of urology or FPMRS providers or that the same provider did not complete the survey more than once. Our survey was likely limited by sampling bias, where those more interested in patient education were more likely to respond. This type of bias would skew the results to appear that more providers are using diverse counseling methods, discussing more content, and utilizing more communication techniques than actually are. Response bias, specifically desirability bias, would also skew the data in this direction as respondents would answer questions in a way that made them look more favorably. In addition, recall bias may have caused providers to report they discussed certain complications and used communication techniques when they did not. Therefore, our data likely overestimates the actual practices of the target provider population.
Our survey was substantially lengthy, with 73 items, to be thorough in characterizing preoperative counseling practices for POP surgery. Although our survey took about five minutes to complete in pretesting, this may have resulted in some nonresponse bias. Our survey could have benefited from a larger sample size with more diversity of provider types. Moreover, we could not ascertain the exact wording utilized during patient counseling and the emphasis placed on symptomatic relief after treatment.
Conclusions
Patient education for POP is a clearly defined challenge for providers. In order to improve patient education delivery, current practices must be identified. Despite its limitations, our survey is the first to characterize the practice patterns of a sample of FPMRS providers, which can guide future studies to develop and implement evidence-based approaches to patient education for POP. Future investigations should evaluate educational preferences from the patient perspective.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-16/rc
Data Sharing Statement: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-16/dss
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-16/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. There’s no human experiments involved, therefore ethic approval or informed consent is not required for this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J 2013;24:1783-90. [Crossref] [PubMed]
- Wu JM, Matthews CA, Conover MM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 2014;123:1201-6. [Crossref] [PubMed]
- Kurkijärvi K, Aaltonen R, Gissler M, et al. Pelvic organ prolapse surgery in Finland from 1987 to 2009: A national register based study. Eur J Obstet Gynecol Reprod Biol 2017;214:71-7. [Crossref] [PubMed]
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002;183:630-41. [Crossref] [PubMed]
- Powell R, Scott NW, Manyande A, et al. Psychological preparation and postoperative outcomes for adults undergoing surgery under general anaesthesia. Cochrane Database Syst Rev 2016;2016:CD008646. [Crossref] [PubMed]
- Jones S, Alnaib M, Kokkinakis M, et al. Pre-operative patient education reduces length of stay after knee joint arthroplasty. Ann R Coll Surg Engl 2011;93:71-5. [Crossref] [PubMed]
- Kenton K, Pham T, Mueller E, et al. Patient preparedness: an important predictor of surgical outcome. Am J Obstet Gynecol 2007;197:654.e1-6. [Crossref] [PubMed]
- Adams SR, Hacker MR, Merport Modest A, et al. Informed consent for sacrocolpopexy: is counseling effective in achieving patient comprehension? Female Pelvic Med Reconstr Surg 2012;18:352-6. [Crossref] [PubMed]
- Pakbaz M, Rolfsman E, Löfgren M. Are women adequately informed before gynaecological surgery? BMC Womens Health 2017;17:68. [Crossref] [PubMed]
- Brach C, Keller D, Hernandez LM, et al. Ten Attributes of Health Literate Health Care Organizations. National Academy of Sciences; 2012.
- Anger JT, Lee UJ, Mittal BM, et al. Health literacy and disease understanding among aging women with pelvic floor disorders. Female Pelvic Med Reconstr Surg 2012;18:340-3. [Crossref] [PubMed]
- Rozier RG, Horowitz AM, Podschun G. Dentist-patient communication techniques used in the United States: the results of a national survey. J Am Dent Assoc 2011;142:518-30. [Crossref] [PubMed]
- Horowitz AM, Wang MQ, Kleinman DV. Opinions of Maryland adults regarding communication practices of dentists and staff. J Health Commun 2012;17:1204-14. [Crossref] [PubMed]
- Corley EM, Terse P, Paulosky KE, et al. Patient Frustration with Pelvic Organ Prolapse Education Met with Resilient Response. Neurourol Urodyn 2022;41:409-15. [Crossref] [PubMed]
- Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ 2007;335:24-7. [Crossref] [PubMed]
- Crabtree TD, Puri V, Bell JM, et al. Outcomes and perception of lung surgery with implementation of a patient video education module: a prospective cohort study. J Am Coll Surg 2012;214:816-21.e2. [Crossref] [PubMed]
- Jeppson PC, Clark MA, Hampton BS, et al. Improving patient knowledge about sacral nerve stimulation using a patient based educational video. J Urol 2013;190:1300-5. [Crossref] [PubMed]
- Kinman CL, Meriwether KV, Powell CM, et al. Use of an iPad™ application in preoperative counseling for pelvic reconstructive surgery: a randomized trial. Int Urogynecol J 2018;29:1289-95. [Crossref] [PubMed]
- Balzarro M, Rubilotta E, Goss C, et al. Counseling in urogynecology: A difficult task, or simply good surgeon-patient communication? Int Urogynecol J 2018;29:943-8. [Crossref] [PubMed]
- Kessels RP. Patients' memory for medical information. J R Soc Med 2003;96:219-22. [PubMed]
- Storms H, Aertgeerts B, Vandenabeele F, et al. General practitioners' predictions of their own patients' health literacy: a cross-sectional study in Belgium. BMJ Open 2019;9:e029357. [Crossref] [PubMed]
- Glaser J, Nouri S, Fernandez A, et al. Interventions to Improve Patient Comprehension in Informed Consent for Medical and Surgical Procedures: An Updated Systematic Review. Med Decis Making 2020;40:119-43. [Crossref] [PubMed]
- The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Published online 2003:76. Available online: https://nces.ed.gov/pubs2006/2006483.pdf
- Du C, Lee W, Lucioni A, et al. Mp02-06 Readability of patient education materials on pelvic organ prolapse, overactive bladder, and stress urinary incontinence. J Urol 2019;201:e12.
- Vijn TW, Fluit CRMG, Kremer JAM, et al. Involving Medical Students in Providing Patient Education for Real Patients: A Scoping Review. J Gen Intern Med 2017;32:1031-43. [Crossref] [PubMed]
Cite this article as: Nemirovsky A, Horowitz AM, Malik RD. Patient counseling for pelvic organ prolapse surgery: methods used for patient education. Gynecol Pelvic Med 2023;6:20.