Use of a modified prone position in transvaginal natural orifice transluminal endoscopic myomectomy: a new surgical technique for posterior uterine myoma
Highlight box
Key findings
• Elucidate a modified prone position that improves patient care during transvaginal natural orifice transluminal endoscopic myomectomy (vNOTEM).
What is known and what is new?
• The lithotomy or Lloyd Davis position are usually chosen for laparoscopic myomectomy.
• The modified prone position is used for transvaginal vNOTEM.
What is the implication, and what should change now?
• Transvaginal vNOTEM with modified prone position is recommended for patients with posterior uterine myoma.
Introduction
Uterine myoma is the most prevalent benign tumor of the female reproductive tract in women of reproductive age (1). It can give rise to various symptoms, including abnormal vaginal bleeding, pelvic pain, and urinary or gastrointestinal symptoms, and may even lead to infertility depending on its size and location. Myomectomy is the standard surgical intervention for patients hoping to preserve uterine fertility (2). The minimally invasive surgeries have been proven to be superior to the traditional laparotomy approach in treating many benign gynecological diseases. Laparoscopic myomectomy has been widely employed for treating uterine myomas over the past few decades. Recent years have witnessed various efforts to further reduce the invasiveness of laparoscopy, resulting in the advent and development of laparoscopic endoscopic single-site surgery (LESS) and natural orifice transluminal endoscopic surgery (NOTES) (3,4). In the pursuit of even greater minimally invasive procedures, the transvaginal route has gained popularity. The utilization of transvaginal natural orifice transluminal endoscopic myomectomy (vNOTEM) has also been reported frequently during recent years (1,5,6).
Given that vNOTEM is performed through the vagina, a 2.0–2.5 cm posterior or anterior colpotomy is required at the beginning of surgical procedure. For myomas situated on or attached to the posterior wall of the uterus, it is evident that the operative space is quite limited when the patient is in the lithotomy or Lloyd Davis position. Additionally, surgeons encounter challenges in cutting, stitching, and knotting under these circumstances. Enhancing maneuverability and facilitating easier cutting and suturing during vNOTEM are critical considerations, which prompted us to adopt a modified prone position for posterior uterine myomas at a tertiary hospital (Chengdu Women’s and Children’s Central Hospital, Chengdu, China), when performing vNOTEM. The objective of this paper is to introduce the application of the modified prone position during vNOTEM for posterior myoma. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-8/rc).
Preoperative preparations and requirements
The selection of candidates for vNOTEM involves strict adherence to specific inclusion and exclusion criteria listed below.
Inclusion criteria:
- Presence of uterine myoma suitable for laparoscopic myomectomy.
- History of sexual intercourse, with or without previous childbirth.
- Willing to undergo vNOTEM.
Exclusion criteria:
- Pelvic inflammation.
- Vaginal inflammation.
- Suspected severe endometriosis or pelvic adhesions.
- Signs indicative of suspected malignant tumors.
- Presence of myoma on the lateral wall.
- Multiple myomas on both the posterior and anterior walls of the uterus.
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
Case report
A 41-year-old patient with a 6 cm solitary posterior uterine myoma met the criteria for transvaginal vNOTEM. The patient’s body mass index (BMI) was 23.2 kg/m2. Having undergone a full-term vaginal delivery and with no history of abdominopelvic surgery, she presented with no preoperative abnormalities. The decision to adopt a prone position for the removal of the posterior myoma in the vNOTEM manner was made. The hospital’s Human Investigation Review Board thoroughly reviewed and approved the technique (Approval No. B202139). Standard preoperative preparations that similar to the traditional laparoscopic surgery were employed, and no intraoperative or postoperative complications occurred.
Video link
Use of a modified prone position in transvaginal vNOTEM for posterior uterine myoma (Video 1). Written consent has been obtained from the patient.
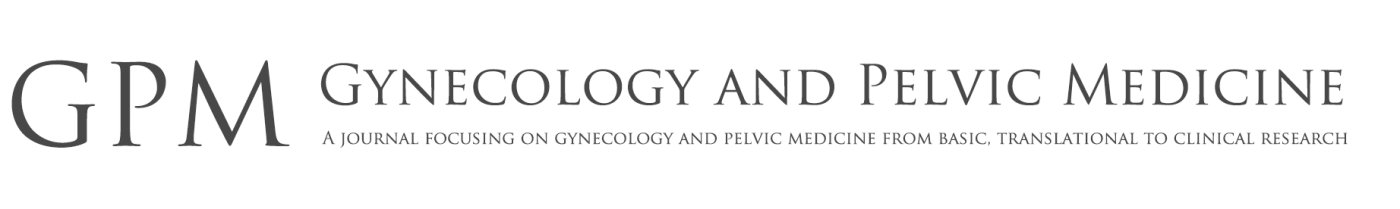
Commencing the procedure, the patient is positioned in a supine posture on a stretcher adjacent to the operating table (Figure 1A). Following the administration of general anesthesia, the stretcher’s height is slightly elevated above that of the operating table. The patient is then carefully maneuvered from a supine position on the stretcher to a prone position, with thighs, elbows, ankles, and knees appropriately supported to alleviate interface pressure (Figure 1B,1C). The anesthesiologist turns the patient’s head to the side, positioning the face on a gel headrest (Figure 1D). Subsequently, a Foley catheter is employed to empty the urinary bladder. Following the completion of skin preparation and draping, the operating table is gradually tilted to a head-down position at the required angles (Figure 2A,2B).
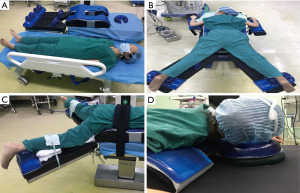
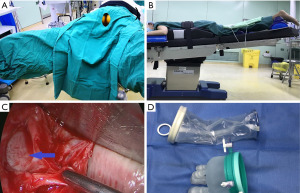
A posterior colpotomy of 2.0–2.5 cm is meticulously made (Figure 2C). The pouch of Douglas is then opened, and a specialized LESS port is inserted through the incision (Figure 2D). The establishment of a pneumoperitoneum ensues. Using the conventional endoscopic instruments and a standard endoscope, the myoma is identified (Figure 3A), and 6 units of vasopressin are injected into the uterine wall (Figure 3B). After the uterine serosa over the myoma become pale, an incision is made (Figure 3C), and the myoma is meticulously resected. Post-enucleation, closure of the myoma bed is performed using a barbed suture, to achieve hemostasis. The excised myoma is carefully extracted through the colpotomy within an endobag. The port is then removed, and the colpotomy is transvaginally closed with a continuous 2-0 barbed suture (Figure 3D).
In circumstances where conversion to conventional laparoscopy becomes inevitable, the patient is repositioned to a supine position, followed by the re-disinfection and re-draping. Upon completion of the surgery, the patient is returned to the supine position on the stretcher for the recovery of general anesthesia. Subsequently, the patient is transferred to the post-anesthesia care unit.
Postoperative considerations and tasks
The patient was carefully monitored for 2–3 days after the surgery. The virginal incision was observed at the day of discharge and one month after surgery. Sexual intercourse was prohibited for at least one month after vNOTEM.
Tips and pearls
The modified prone position is not difficult to implement and requires no specialized qualifications. However, experienced laparoscopists are recommended to perform the vNOTEM. Additionally, attention should be paid to the following points to prevent neural and musculoskeletal injuries: (I) special care must be taken to avoid pressure on the patient’s eyes or nose; (II) The shoulder should be abducted by less than 90˚, and a 15–20˚ head-down tilt is usually sufficient for the surgical procedure.
The most crucial surgical step is establishing the surgical platform for vNOTEM. Rectal injury may occur when cutting the posterior vaginal fornix, especially in the presence of adhesions in the pouch of Douglas. Therefore, detailed preoperative examinations and proper patient selection are crucial.
Dealing with adhesions and bleeding is also a key aspect of the operation. The skill of dissecting adhesions is akin to conventional laparoscopy. The injection of vasopressin before cutting and the use of barbed sutures can minimize bleeding.
The recommended inclusion criteria are as follows: mandatory laparoendoscopy for treating solitary posterior myoma, and preoperative examinations showing a low probability of malignancy. Exclusion criteria involve a history of rectal surgery, severe pelvic inflammatory disease, pelvic radiotherapy, suspected or confirmed rectovaginal endometriosis, confirmed severe pelvic adhesion, and no history of sexual intercourse.
Discussion
Recently, transvaginal natural orifice transluminal endoscopic surgery (vNOTES) has emerged as a new concept in minimally invasive surgery, particularly in gynecology (3). vNOTEM for uterine myoma has been invented recently and gained increasing popularity. Adequate exposure of the lesion is a precondition for a successful surgery, and good exposure can reduce the duration of the operation, subsequently minimizing complications.
Two published articles have enrolled posterior uterine myoma cases. Baekelandt J presented a case series of eight women undergoing vNOTEM, although the surgical position was not explicitly mentioned (6). Lee et al. reported three cases of women undergoing vNOTEM in 2014, and the authors opted for the Lloyd-Davies position (head-down lithotomy) for the three patients with solitary posterior uterine leiomyoma (5). The authors noted a potentially increased risk due to relatively restricted vision with this position (5). The rationale for not using the common lithotomy/Lloyd Davis position in vNOTEM for posterior uterine myoma is the surgeon’s need for optimal vision. Placing female patients in a prone position with separated legs, especially with the head down, offers superior exposure of the posterior uterine wall. Additionally, the surgeon can more easily incise and suture the posterior uterine wall in the prone position.
It is essential to acknowledge that operative positions can affect the patient’s physiology. Achieving optimal surgical positioning requires balancing the need for good surgical access with minimal risks to the patient, such as hemodynamic instability, impaired ventilation, and neural or musculoskeletal injury. In our preliminary practice, the modified prone position has not been associated with major cardiovascular, respiratory derangements, or neural injuries intraoperatively.
Noteworthily, for this surgical technique, the surgeon is not able to visualize or operate on the anterior or lateral wall of the uterus. Therefore, this technique is only suitable for the excision of posterior uterine myoma.
Conclusions
We introduced the vNOTEM approach with the modified prone position for patients with posterior uterine myoma, which enhances the optimization of surgical care for patients with posterior uterine myoma.
Acknowledgments
The video was awarded the second prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-8/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-8/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-8/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu J, Lin Q, Blazek K, et al. Transvaginal Natural Orifice Transluminal Endoscopic Surgery Myomectomy: A Novel Route for Uterine Myoma Removal. J Minim Invasive Gynecol 2018;25:959-60. [Crossref] [PubMed]
- Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril 2009;91:1215-23. [Crossref] [PubMed]
- Yoshiki N. Review of transvaginal natural orifice transluminal endoscopic surgery in gynecology. Gynecol Minim Invasive Ther 2017;6:1-5. [Crossref] [PubMed]
- Li CB, Hua KQ. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgeries: A systematic review. Asian J Surg 2020;43:44-51. [Crossref] [PubMed]
- Lee CL, Huang CY, Wu KY, et al. Natural orifice transvaginal endoscopic surgery myomectomy: an innovative approach to myomectomy. Gynecol Minim Invasive Ther 2014;3:127-30. [Crossref]
- Baekelandt J. Transvaginal natural-orifice transluminal endoscopic surgery: a new approach to myomectomy. Fertil Steril 2018;109:179. [Crossref] [PubMed]
Cite this article as: Feng D, He L, Lin Y. Use of a modified prone position in transvaginal natural orifice transluminal endoscopic myomectomy: a new surgical technique for posterior uterine myoma. Gynecol Pelvic Med 2023;6:23.