A case of stage IB1 cervical cancer radical hysterectomy by fluorescent laparoscopic navigation combined with indocyanine green (ICG) sentinel lymph node excision
Introduction
Cervical cancer ranks fourth in the world in female malignancies. In 2015, about 270,000 patients died, 90% of which occurred in low- and middle-income countries (LMIC), with a mortality rate about 18 times greater than developed countries (1). The results of most previous studies on the treatment of cervical cancer are similar, and it is believed that laparoscopic surgery and open surgery have the same efficacy, and laparoscopic surgery has a short hospital stay, less blood loss, faster recovery time and fewer postoperative complications. Last year, one prominent study showed a comparison of routine surgical options for early cervical cancer (2). It was found that minimally invasive radical hysterectomy had a higher recurrence rate and a lower survival rate than open abdominal radical hysterectomy, which can be described as shocking and subversive. Since laparoscopic surgery is widely used in Mainland China, Chinese obstetrics and gynecology experts designed the study to follow Ramirez, who did the laparoscopic and open surgery as a true world study on early cervical cancer and found that we should continue to improve the operation and the technology of laparoscopic surgery.
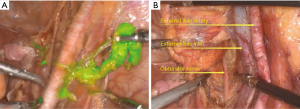
Here, we performed fluorescent laparoscopic sentinel lymph node biopsy and radical cervical cancer resection in a woman diagnosed with stage IB1 cervical cancer (3) (Figure 1).
Operative techniques
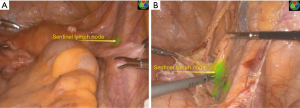
For this patient, we performed radical cervical cancer hysterectomy with the laparoscopic multi-hole method and sentinel node removal with fluorescent laparoscopy. Sentinel lymph node is the first station of lymph node metastasis, and it is also the earliest metastasis lymph nodes. First, 0.5 mL ICG was injected into the cervical clockwise clock at 3 and 9 o’clock after a conventional disinfection towel. After 5 minutes, bilateral internal iliac lymph nodes were developed first (Figure 2A), the right side of the peritoneum was opened, and the sentinel lymph nodes developed at the intersection of the external iliac, and internal iliac vessels were removed (Figure 2B). Similarly, the left internal iliac sentinel node was taken for biopsy.
Pelvic lymph node dissection
Currently, for cervical cancer patients with negative sentinel lymph node biopsy, no literature has reported that systematic lymph nodes can be left unexcised. Even in the case of negative sentinel lymph node biopsy, systematic pelvic lymph node dissection was performed for patients (Figure 3A,B).
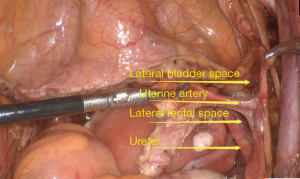
Uterine arteries ligation
The key to uterine artery ligation is to identify its anatomical location and dissociate it (Figure 4).
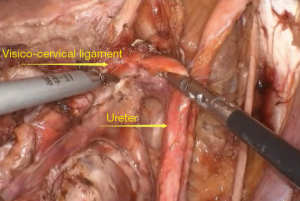
Ureter separation
The ureter is an especially important structure in radical cervical cancer surgery. Its dissociation and protection is the key to extensive total hysterectomy (Figure 5).
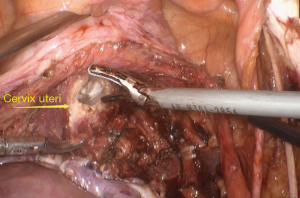
Break off the cervix uteri
No uterine manipulator was used during the entire procedure of a broad hysterectomy, and it is entirely dependent on the coordination between the assistant and the doctor. During cervix removal, a condom is inserted into the vagina to prevent gas leakage from the abdominal cavity (Figures 6,7).
Comments
Lymph node metastasis is an important predictor of recurrence and prognosis of cervical cancer. Given the importance of lymph node metastasis, it is of considerable significance to explore preoperative prediction, exact intraoperative location, and judgment of retroperitoneal lymph node metastasis by using ICG for lymph node development. In this paper, the sentinel lymph node biopsy was performed in patients with cervical squamous cell carcinoma, which can be used to guide the feasibility of lymph node resection and predict the clinical value of lymph node metastasis. Then, no uterine manipulator was used during the operation. Cervical cancer cells can spread and metastasize when the lifting device is inserted into the uterus, which can be difficult to detect (5).
Acknowledgments
The video was awarded the third prize in the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery).
Funding: The present study was sponsored by the National Natural Science Foundation of China (No. 81972425), the Shanghai PuJiang Program (No. 17PJD032) and the Project Young Elite of the Shanghai Health System (No. 2017YQ063).
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm.2019.12.02/coif). The series “Award-Winning Videos from the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med 2018;379:1895-904. [Crossref] [PubMed]
- Cohen PA, Jhingran A, Oaknin A, et al. Cervical cancer. Lancet 2019;393:169-82. [Crossref] [PubMed]
- Bhatla N, Berek JS, Cuello Fredes M, et al. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet 2019;145:129-35. [Crossref] [PubMed]
- Zhou X, Zhang R, Wu C, et al. This video shows a fluoroscopic laparoscopic sentinel lymph node biopsy and an extensive total hysterectomy without a uterine manipulator. Asvide 2019;6:349. Available online: http://www.asvide.com/watch/33034
- Melamed A, Margul DJ, Chen L, et al. Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. N Engl J Med 2018;379:1905-14. [Crossref] [PubMed]
Cite this article as: Zhou X, Zhang R, Wu C, Bao W, Zhu Y. A case of stage IB1 cervical cancer radical hysterectomy by fluorescent laparoscopic navigation combined with indocyanine green (ICG) sentinel lymph node excision. Gynecol Pelvic Med 2019;2:30.