预防子宫内膜异位症复发的激素治疗
背景介绍
子宫内膜异位症是子宫内膜腺体和间质出现在子宫内膜以外的部位引起的一种慢性疾病。大约10%的育龄期妇女和33%-50%的慢性盆腔痛和/或不育妇女受该疾病影响[1-3]。这种情况在东亚种族中普遍存在,而非裔美国人受到的影响较小[4]。遗传、表型和生活方式似乎是影响子宫内膜异位和子宫内膜异位症的多因素病因[5]。
卵巢是异位组织最常见的植入部位,子宫内膜异位囊肿是该病的经典表型之一[6]。囊肿常见于单侧,更倾向于左侧[7]。
子宫内膜异位的发病机制是多因素的,不能由单一的致病理论来解释[8]。已经提出了几种假说,其中包括原位理论和移植理论:第一种是认为子宫内膜异位症的发生,由卵巢生殖上皮的化生或中胚层和苗勒氏残余的胚胎起源引起[9-11]。相反,移植理论认为子宫内膜异位病变可能是月经期间子宫内膜异位组织通过输卵管流入腹腔引起。为了支持经血逆流理论和腹腔液体运动的作用,子宫内膜异位症的左易位性可以通过乙状结肠的解剖屏障来解释,该解剖屏障可能会延迟子宫内膜异位组织从左半盆的清除并促进在卵巢种植[12-14]。
遗传和后天的几种机制都可能影响子宫内膜异位症的发展。在子宫内膜异位症患者中观察到,大量基因再加上控制免疫学、组织学和生物学变化的表观遗传现象,似乎具有共同的作用[8]。一些责任基因调节雌激素受体的表达以及循环雌激素和孕激素的血清水平[15]。高雌激素水平和雌激素受体β(ERβ)的过表达,以及子宫内膜异位组织中ERα与ERβ比率的倒置,似乎都支持基于雌激素的异位细胞的存活。此外,考虑到孕激素对雌激素反应的调节作用,在受影响的妇女中发现孕激素抵抗在维持这种失调的激素环境中起着协同作用[16,17]。
经阴道超声检查是诊断子宫内膜异位症的一种方法,具有很高的敏感性和特异性。子宫内膜异位症的典型超声特征是具有“毛玻璃”的均质性、低回声和血供差的单房囊肿。子宫内膜异位症的外科和/或药物疗法旨在控制症状(尤其是慢性盆腔痛和痛经)并预防囊肿的生长;药物治疗可降低手术后的复发率。不幸的是,研究报道子宫内膜异位症的术后复发率很高,高达30%到40%,这让妇科医生在管理这种慢性疾病时感到沮丧[6,20-25]。
对已经存在的子宫内膜异位症没有有效的药物治疗方法,因此,为了预防疾病复发并最大程度地降低卵巢储备功能受损的风险,在手术切除后进行包括药物辅助治疗在内的三级预防,对于将来希望受孕的女性尤为重要[26-29]。此外,考虑到疾病复发的速度,应在囊肿切除术后不久就开始药物治疗[30]。
据报道,长效抑制性激素治疗在预防子宫内膜异位症的复发中起着至关重要的作用[31]。一些激素替代治疗已经应用于临床实践,例如口服避孕药(OC)、孕激素(PG)、促性腺激素释放激素类似物(GnRHa)、达那唑、芳香化酶抑制剂(AI)、GnRH拮抗剂、选择性雌激素受体调节剂(SERM)和选择性孕激素受体调节剂(SPRM)[32,33]。除激素疗法外,还研究了替代性植物疗法,例如药用植物,植物化学物质和多组分草药制剂,已经获得了可喜的结果。实际上,其中一些化合物似乎会影响表观遗传因素、细胞凋亡、细胞存活以及血管生成过程和氧化应激。此外,特定药物在雌激素调节中也有作用[34-36]。
然而,激素治疗仍然是治疗子宫内膜异位相关疼痛最常用的选择,因此光线疗法仅限于科学研究的范围。抑制排卵和减少经血逆流是疾病发展的关键因素,这是OC和PG发挥作用的潜在机制。由于成本低和安全性高,这些是子宫内膜异位症最常用的治疗药物[37-39]。如果患者没有生育需求,则应规律服用这些药物作为长期治疗方案。如果连续给药,这些药物可导致闭经,能完全解决痛经和避免经血逆行[31,40]。在这种情况下,可使用左炔诺孕酮宫内缓释系统(LNG-IUS)。这个装置不会抑制排卵(植入几个月后除外),但是它能使月经减少或消失[41,42]。
GnRHa是另一个广泛使用的药物,对减少子宫内膜异位症术后的疼痛和复发有有益的影响。然而,它更昂贵,且因为有与严重的低雌激素水平有关的副作用,例如潮红、泌尿生殖器萎缩、性欲减退、血脂代谢恶化、抑郁和骨质流失,患者耐受性差。因此,GnRHa通常与“反向添加”疗法(包括醋酸炔诺酮、小剂量雌孕激素替代疗法、OC和双膦酸盐)联合使用[33,43]。关于AI、GnRH拮抗剂和达那唑在子宫内膜异位症治疗中的影响,目前尚无可用数据[44,45]。本文旨在评估辅助激素治疗在预防子宫内膜异位症术后复发的疗效。
手术技巧
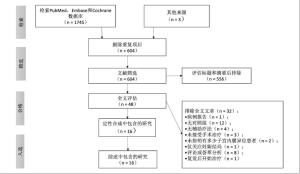
在本篇综述中,我们在PubMed、Embase和Cochrane数据库系统检索了有关预防子宫内膜异位症术后复发激素治疗的相关研究,并使用了以下关键词:“子宫内膜异位症复发”、“激素治疗”、“辅助疗法”、“子宫内膜异位症切除”、“ GnRH激动剂”、“口服避孕药”、“孕激素”、“左炔诺孕酮宫内缓释系统”、“达那唑”、“芳香化酶抑制剂”。检索是由两位作者完成的,首先阅读标题和摘要,然后阅读全文。
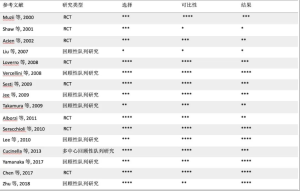
我们纳入了符合以下标准的研究:随机对照试验(RCT)或队列研究,有对照组或安慰剂组和接受子宫内膜异位症手术治疗和辅助激素治疗的研究组,报告了子宫内膜异位症复发率同时用英文发表的研究。我们排除了病例报告、综述或荟萃分析、以摘要形式发表的研究、由子宫内膜异位患者组成的研究组(未指明是否患有卵巢子宫内膜异位症)以及仅在结果中报告妊娠结局的研究。经验证的量表(纽卡斯尔-渥太华量表)用于所纳入研究的质量评估(表S1)。
Full table
结果
研究选择
对Medline和其他来源的系统检索确定了1,748项研究,并纳入了48篇文章进行评估。我们排除了一项研究,因为这是一例病例报告[45],其中12项研究没有对照组[24,46-56],四项研究未在术后进行激素治疗[22,57-59],三项研究是由于患者未接受子宫内膜异位症的外科手术治疗[44,60,61],两项研究未明确说明子宫内膜异位症的患者是否有卵巢子宫内膜异位囊肿[62,63],一项研究未报告子宫内膜异位症复发率(仅关注妊娠结局)[64],八项研究是评论或荟萃分析[31,39,43,65-69],一项研究是因为子宫内膜异位症复发后才开始进行激素治疗[70]。最后,从16篇文章中提取了评估激素治疗对子宫内膜异位症预防效果的数据,其中8篇是RCT[71-78],另外8篇是队列研究[6,25,79-84]。筛选研究的过程如图1所示。
研究描述和结果总结
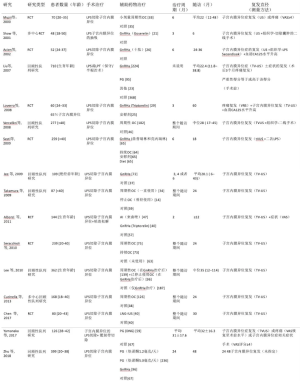
表1总结了本综述中所包括研究的主要细节和设计。六项研究评估了腹腔镜切除囊肿后OC对子宫内膜异位症复发的影响[25,71,76,80-82],四项研究研究报告了辅助性GnRHa治疗的效果[72-74,79],另外两项将GnRHa与PG进行了比较[6,84],一篇将GnRHa与OC进行了比较[75],另一篇将GnRHa与AI进行了比较[77],其中一个研究了PG的疗效[83],另一个研究了LNG-IUS[78]的作用。所有研究均包含对照组或安慰剂组。只有六项研究[25,76,80-83]的治疗时间与随访时间相吻合,而其他研究的治疗时间较短。
Full table
几乎所有纳入的研究都通过超声检查评估子宫内膜异位症的复发(Zhu等的研究并未明确阐述子宫内膜异位症复发的评估方法[84]),其中一些研究还认为症状[6,71,74,78,83]或血清CA125水平升高[73,74,78]是疾病复发的标志。很少有研究报道子宫内膜异位囊肿的复发由手术和组织学得以证实[25,72,73,75]。
关于复发率(表2),七项研究报告了术后激素治疗预防子宫内膜异位症复发的优势[25,72,76,80-83]。在这些研究中,Shaw等的RCT[72]与其他研究的可比性很差(表S1),因为该疗法是对子宫内膜异位囊肿进行手术抽吸(而非切除)后进行的。该作者报告说,仅使用戈斯瑞林三个月就可以减小子宫内膜异位症的大小,为二线手术治疗提供了潜在的优势。Seracchioli等[76]发现囊肿复发的平均直径每6个月会增加,与周期性OC使用者(0.31±0.18 cm)和连续OC使用者 (0.25±0.09厘米)相比,尤其是对照组(非使用者OC)(0.48±0.3 cm)增加更多。
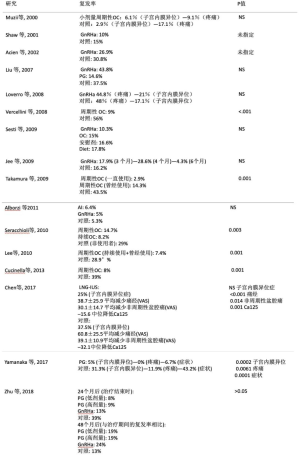
Full table
Cucinella等[82]将对照组(拒绝辅助治疗的妇女)与周期性OC使用者进行了比较,根据不同的孕激素类型(单相去氧孕烯,单相孕二烯和双相孕烯醇)将周期性OC使用者分为三个亚组。他们观察到非使用者中囊肿复发的累积概率为74.7%,而其他三个亚组中风险极低,分别为26.5%,31.8%和20.5%。与非使用者(3.1 cm; P = 0.0001)相比,使用者中复发性子宫内膜异位囊肿的平均直径相比更小(分别为1.9、1.8、1.3 cm)。
其他研究人员[83]对126例子宫内膜异位囊肿和深层浸润性子宫内膜异位症患者进行研究,探索了地诺孕素(DNG)对周期性疼痛和子宫内膜异位症的影响。他们观察到与对照组相比,治疗后子宫内膜异位症相关的疼痛和子宫内膜异位症明显缓解。但是,在其他与子宫内膜异位症相关的症状(痛经、非经期骨盆痛、痛经和性交困难)上,除痛经外,DNG使用者与非使用者之间没有统计学上的显着差异(P <0.001)。
最后,有五项研究报告术后激素治疗在预防子宫内膜异位复发方面没有任何优势[71,73-75,77]。本研究中包括的其他研究则是结果不一致或结论不同。研究对象最多的研究[6](710名妇女)对于术后激素治疗是否有益尚无定论(P值无统计学意义);而据其报告,其他因素与复发更有相关性(既往药物使用、既往手术、美国生育协会修订总评分和手术年龄较小)。
Jee等[79]报告了不同的结果。他们将三种不同的GnRHa治疗持续时间(3、4和6个月)与对照组进行了比较,仅在治疗6个月后观察到较低的复发率,而治疗时间较短或不做任何治疗,对卵巢子宫内膜异位囊肿的传统腹腔镜手术后的复发率没有有益的影响。
讨论
基于激素治疗短期使用(最长6个月)和治疗结束后几个月对囊肿复发进行超声评估,五项研究[71,73-75,77]报告辅助治疗在子宫内膜异位症复发方面无益。尽管有相同的治疗时间和随访时间(30个月),但只有一项研究[78]报告辅助治疗无有益作用。这项研究是本评价中唯一评估LNG-IUS作为辅助治疗的研究。但是,该结果与有关术后使用LNG-IUS的其他研究不一致(由于没有对照组而未包括在内)。Taneja等[54]比较了LNG-IUS和达那唑,报告指出LNG-IUS在缓解疼痛和预防复发方面更有效(65.2%对38.0%,P <0.05)。相反,Cho等[52]发现术后使用LNG-IUS和周期性OC在预防子宫内膜异位症复发方面无显著差异(P = 0.461)。其他研究者[48]将醋酸甲羟孕酮与LNG-IUS进行了比较,但未观察到两组子宫内膜异位症复发率有显著差异。此外,这些作者认为,LNG-IUS组的依从性更好,对症状控制和预防复发具有有益作用。其余所有在随访期间持续治疗的研究均观察到术后激素疗法具有优势[25,76,80-83]。
Zhu等的回顾性队列研究[84]是唯一报道12个月后(药物治疗结束时)和24个月后(药物治疗结束后12个月)子宫内膜异位症复发率的研究。在第一年后,对照组显示出更高的复发率,而在暂停治疗后医学上的有益作用似乎不那么重要。
结论
即使一些研究报告了相互矛盾的结果,几种激素化合物,例如OC、PG和GnRHa已被证明对子宫内膜异位症复发有益。目前尚不清楚在预防子宫内膜异位症复发方面,一种激素治疗是否优于其他激素治疗。但是,辅助治疗的持续时间似乎具有至关重要的作用。关于达那唑、AI、SERM和SPRMS在术后期间的作用的研究仍然很少,还需要其他证据来阐明哪种激素治疗可能是最佳选择。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Medical Therapy in Endometriosis Treatment”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-20-23/coif). The series “Medical Therapy in Endometriosis Treatment” was commissioned by the editorial office without any funding or sponsorship. FB served as an unpaid Guest Editor of the series. SF served as an unpaid Guest Editor of the series and serves as an editorial board member of Gynecology and Pelvic Medicine from Oct 2018 to Sept 2020. The authors have no other conflicts of interest to declare.
Ethical statement: The authors are accountable for all aspects of this work in ensuring that questions related to the accuracy or integrity of any part of this work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Giudice LC, Kao LC. Endometriosis. Lancet 2004;364:1789-99. [Crossref] [PubMed]
- Meuleman C, Vandenabeele B, Fieuws S, et al. High prevalence of endometriosis in infertile women with normal ovulation and normospermic partners. Fertil Steril 2009;92:68-74. [Crossref] [PubMed]
- Ferrero S, Arena E, Morando A, et al. Prevalence of newly diagnosed endometriosis in women attending the general practitioner. Int J Gynaecol Obstet 2010;110:203-7. [Crossref] [PubMed]
- Missmer SA, Cramer DW. The epidemiology of endometriosis. Obstet Gynecol Clin North Am 2003;30:1-19. vii. [Crossref] [PubMed]
- Ozkan S, Murk W, Arici A. Endometriosis and infertility: epidemiology and evidence-based treatments. Ann N Y Acad Sci 2008;1127:92-100. [Crossref] [PubMed]
- Liu X, Yuan L, Shen F, et al. Patterns of and risk factors for recurrence in women with ovarian endometriomas. Obstet Gynecol 2007;109:1411-20. [Crossref] [PubMed]
- Ferrero S, Ragni N, Fulcheri E. Lateral distribution of benign ovarian cysts. Int J Gynaecol Obstet 2005;89:150-1. [Crossref] [PubMed]
- Laganà AS, Garzon S, Götte M, et al. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int J Mol Sci 2019;20:5615. [Crossref] [PubMed]
- Lauchlan SC. The secondary Mullerian system. Obstet Gynecol Surv 1972;27:133-46. [Crossref] [PubMed]
- Batt RE, Yeh J. Mullerianosis: four developmental (embryonic) mullerian diseases. Reprod Sci 2013;20:1030-7. [Crossref] [PubMed]
- van der Linden PJ. Theories on the pathogenesis of endometriosis. Hum Reprod 1996;11:53-65. [Crossref] [PubMed]
- Ulukus M, Yeniel AO, Ergenoglu AM, et al. Right endometrioma is related with more extensive obliteration of the Douglas pouch. Arch Gynecol Obstet 2012;285:1483-6. [Crossref] [PubMed]
- Bricou A, Batt RE, Chapron C. Peritoneal fluid flow influences anatomical distribution of endometriotic lesions: why Sampson seems to be right. Eur J Obstet Gynecol Reprod Biol 2008;138:127-34. [Crossref] [PubMed]
- Vercellini P, Pisacreta A, Vicentini S, et al. Lateral distribution of nonendometriotic benign ovarian cysts. BJOG 2000;107:556-8. [Crossref] [PubMed]
- Maruyama T, Yoshimura Y. Molecular and cellular mechanisms for differentiation and regeneration of the uterine endometrium. Endocr J 2008;55:795-810. [Crossref] [PubMed]
- McKinnon B, Mueller M, Montgomery G. Progesterone Resistance in Endometriosis: an Acquired Property? Trends Endocrinol Metab 2018;29:535-48. [Crossref] [PubMed]
- Bulun SE, Monsavais D, Pavone ME, et al. Role of estrogen receptor-beta in endometriosis. Semin Reprod Med 2012;30:39-45. [Crossref] [PubMed]
- Endometriosis Treatment Italian Club. Ovarian endometrioma: what the patient needs. J Minim Invasive Gynecol 2014;21:505-16. [Crossref] [PubMed]
- Guerriero S, Ajossa S, Mais V, et al. The diagnosis of endometriomas using colour Doppler energy imaging. Hum Reprod 1998;13:1691-5. [Crossref] [PubMed]
- Kim ML, Kim JM, Seong SJ, et al. Recurrence of ovarian endometrioma after second-line, conservative, laparoscopic cyst enucleation. Am J Obstet Gynecol 2014;210:216.e1-6. [Crossref] [PubMed]
- Vercellini P, Somigliana E, Vigano P, et al. Endometriosis: current therapies and new pharmacological developments. Drugs 2009;69:649-75. [Crossref] [PubMed]
- Kikuchi I, Takeuchi H, Kitade M, et al. Recurrence rate of endometriomas following a laparoscopic cystectomy. Acta Obstet Gynecol Scand 2006;85:1120-4. [Crossref] [PubMed]
- Busacca M, Chiaffarino F, Candiani M, et al. Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am J Obstet Gynecol 2006;195:426-32. [Crossref] [PubMed]
- Koga K, Takemura Y, Osuga Y, et al. Recurrence of ovarian endometrioma after laparoscopic excision. Hum Reprod 2006;21:2171-4. [Crossref] [PubMed]
- Vercellini P, Somigliana E, Daguati R, et al. Postoperative oral contraceptive exposure and risk of endometrioma recurrence. Am J Obstet Gynecol 2008;198:504.e1-5. [Crossref] [PubMed]
- Ferrero S, Evangelisti G, Barra F. Current and emerging treatment options for endometriosis. Expert Opin Pharmacother 2018;19:1109-25. [Crossref] [PubMed]
- Leone Roberti Maggiore U, Gupta JK, Ferrero S. Treatment of endometrioma for improving fertility. Eur J Obstet Gynecol Reprod Biol 2017;209:81-5. [Crossref] [PubMed]
- Tafi E, Leone Roberti Maggiore U, Alessandri F, et al. Advances in pharmacotherapy for treating endometriosis. Expert Opin Pharmacother 2015;16:2465-83. [Crossref] [PubMed]
- Ferrero S, Alessandri F, Racca A, et al. Treatment of pain associated with deep endometriosis: alternatives and evidence. Fertil Steril 2015;104:771-92. [Crossref] [PubMed]
- Falcone T, Flyckt R. Clinical Management of Endometriosis. Obstet Gynecol 2018;131:557-71. [Crossref] [PubMed]
- Somigliana E, Vercellini P, Vigano P, et al. Postoperative medical therapy after surgical treatment of endometriosis: from adjuvant therapy to tertiary prevention. J Minim Invasive Gynecol 2014;21:328-34. [Crossref] [PubMed]
- Barra F, Grandi G, Tantari M, et al. A comprehensive review of hormonal and biological therapies for endometriosis: latest developments. Expert Opin Biol Ther 2019;19:343-60. [Crossref] [PubMed]
- Platteeuw L, D'Hooghe T. Novel agents for the medical treatment of endometriosis. Curr Opin Obstet Gynecol 2014;26:243-52. [Crossref] [PubMed]
- Scutiero G, Iannone P, Bernardi G, et al. Oxidative Stress and Endometriosis: A Systematic Review of the Literature. Oxid Med Cell Longev 2017;2017:7265238 [Crossref] [PubMed]
- Taniguchi F, Kaponis A, Izawa M, et al. Apoptosis and endometriosis. Front Biosci (Elite Ed) 2011;3:648-62. [Crossref] [PubMed]
- Della Corte L, Noventa M, Ciebiera M, et al. Phytotherapy in endometriosis: an up-to-date review. J Complement Integr Med 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Leyland N, Casper R, Laberge P, et al. Endometriosis: diagnosis and management. J Obstet Gynaecol Can 2010;32:S1-32. [Crossref] [PubMed]
- . Practice bulletin no. 114: management of endometriosis. Obstet Gynecol 2010;116:223-36. [Crossref] [PubMed]
- Vercellini P, DE, Matteis S, Somigliana E, et al. Long-term adjuvant therapy for the prevention of postoperative endometrioma recurrence: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2013;92:8-16. [Crossref] [PubMed]
- Dunselman GA, Vermeulen N, Becker C, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod 2014;29:400-12. [Crossref] [PubMed]
- Barra F, Scala C, Ferrero S. Current understanding on pharmacokinetics, clinical efficacy and safety of progestins for treating pain associated to endometriosis. Expert Opin Drug Metab Toxicol 2018;14:399-415. [Crossref] [PubMed]
- Muzii L. Medicated intrauterine systems for treatment of endometriosis-associated pain. J Minim Invasive Gynecol 2006;13:535-8. [Crossref] [PubMed]
- Rehmer JM, Flyckt RL, Goodman LR, et al. Management of Endometriomas. Obstet Gynecol Surv 2019;74:232-40. [Crossref] [PubMed]
- Agarwal SK, Foster WG. Reduction in Endometrioma Size with Three Months of Aromatase Inhibition and Progestin Add-Back. Biomed Res Int 2015;2015:878517 [Crossref] [PubMed]
- Lall Seal S, Kamilya G, Mukherji J, et al. Aromatase inhibitors in recurrent ovarian endometriomas: report of five cases with literature review. Fertil Steril 2011;95:291.e15-8. [PubMed]
- Donnez J, Nisolle M, Gillet N, et al. Large ovarian endometriomas. Hum Reprod 1996;11:641-6. [Crossref] [PubMed]
- Park HJ, Koo YA, Yoon BK, et al. Postoperative long-term maintenance therapy with oral contraceptives after gonadotropin-releasing hormone analog treatment in women with ovarian endometrioma. J Minim Invasive Gynecol 2009;16:34-9. [Crossref] [PubMed]
- Wong AY, Tang LC, Chin RK. Levonorgestrel-releasing intrauterine system (Mirena) and Depot medroxyprogesterone acetate (Depoprovera) as long-term maintenance therapy for patients with moderate and severe endometriosis: a randomised controlled trial. Aust N Z J Obstet Gynaecol 2010;50:273-9. [Crossref] [PubMed]
- Muzii L, Maneschi F, Marana R, et al. Oral estroprogestins after laparoscopic surgery to excise endometriomas: continuous or cyclic administration? Results of a multicenter randomized study. J Minim Invasive Gynecol 2011;18:173-8. [Crossref] [PubMed]
- Muneyyirci-Delale O, Anopa J, Charles C, et al. Medical management of recurrent endometrioma with long-term norethindrone acetate. Int J Womens Health 2012;4:149-54. [Crossref] [PubMed]
- Vlahos N, Vlachos A, Triantafyllidou O, et al. Continuous versus cyclic use of oral contraceptives after surgery for symptomatic endometriosis: a prospective cohort study. Fertil Steril 2013;100:1337-42. [Crossref] [PubMed]
- Cho S, Jung JA, Lee Y, et al. Postoperative levonorgestrel-releasing intrauterine system versus oral contraceptives after gonadotropin-releasing hormone agonist treatment for preventing endometrioma recurrence. Acta Obstet Gynecol Scand 2014;93:38-44. [Crossref] [PubMed]
- Kim ML, Cho YJ, Kim MK, et al. The efficacy of long-term maintenance therapy with a levonorgestrel-releasing intrauterine system for prevention of ovarian endometrioma recurrence. Int J Gynaecol Obstet 2016;134:256-9. [Crossref] [PubMed]
- Taneja A, Kaur S, Soni RK, et al. Evaluating the Efficacy of Levonorgestrel Intrauterine System and Danazol for Relief of Postoperative Pain in Endometriosis. J Clin Diagn Res 2017;11:QC10-2. [PubMed]
- Seo JW, Lee DY, Kim SE, et al. Comparison of long-term use of combined oral contraceptive after gonadotropin-releasing hormone agonist plus add-back therapy versus dienogest to prevent recurrence of ovarian endometrioma after surgery. Eur J Obstet Gynecol Reprod Biol 2019;236:53-7. [Crossref] [PubMed]
- Angioni S, Pontis A, Malune ME, et al. Is dienogest the best medical treatment for ovarian endometriomas? Results of a multicentric case control study. Gynecol Endocrinol 2020;36:84-6. [Crossref] [PubMed]
- Kavoussi SK, Odenwald KC, As-Sanie S, et al. Incidence of ovarian endometrioma among women with peritoneal endometriosis with and without a history of hormonal contraceptive use. Eur J Obstet Gynecol Reprod Biol 2017;215:220-3. [Crossref] [PubMed]
- Tsujioka H, Inoue Y, Emoto M, et al. The efficacy of preoperative hormonal therapy before laparoscopic cystectomy of ovarian endometriomas. J Obstet Gynaecol Res 2009;35:782-6. [Crossref] [PubMed]
- Westhoff C, Britton JA, Gammon MD, et al. Oral contraceptive and benign ovarian tumors. Am J Epidemiol 2000;152:242-6. [Crossref] [PubMed]
- Del Forno S, Mabrouk M, Arena A, et al. Dienogest or Norethindrone acetate for the treatment of ovarian endometriomas: Can we avoid surgery? Eur J Obstet Gynecol Reprod Biol 2019;238:120-4. [Crossref] [PubMed]
- Harada T, Momoeda M, Taketani Y, et al. Low-dose oral contraceptive pill for dysmenorrhea associated with endometriosis: a placebo-controlled, double-blind, randomized trial. Fertil Steril 2008;90:1583-8. [Crossref] [PubMed]
- Morelli M, Sacchinelli A, Venturella R, et al. Postoperative administration of dienogest plus estradiol valerate versus levonorgestrel-releasing intrauterine device for prevention of pain relapse and disease recurrence in endometriosis patients. J Obstet Gynaecol Res 2013;39:985-90. [Crossref] [PubMed]
- Tanmahasamut P, Rattanachaiyanont M, Angsuwathana S, et al. Postoperative levonorgestrel-releasing intrauterine system for pelvic endometriosis-related pain: a randomized controlled trial. Obstet Gynecol 2012;119:519-26. [Crossref] [PubMed]
- Kolanska K, Cohen J, Bendifallah S, et al. Pregnancy outcomes after controlled ovarian hyperstimulation in women with endometriosis-associated infertility: GnRH-agonist versus GnRH-antagonist. J Gynecol Obstet Hum Reprod 2017;46:681-6. [Crossref] [PubMed]
- Song SY, Park M, Lee GW, et al. Efficacy of levonorgestrel releasing intrauterine system as a postoperative maintenance therapy of endometriosis: A meta-analysis. Eur J Obstet Gynecol Reprod Biol 2018;231:85-92. [Crossref] [PubMed]
- Zheng Q, Mao H, Xu Y, et al. Can postoperative GnRH agonist treatment prevent endometriosis recurrence? A meta-analysis. Arch Gynecol Obstet 2016;294:201-7. [Crossref] [PubMed]
- Seracchioli R, Mabrouk M, Manuzzi L, et al. Post-operative use of oral contraceptive pills for prevention of anatomical relapse or symptom-recurrence after conservative surgery for endometriosis. Hum Reprod 2009;24:2729-35. [Crossref] [PubMed]
- Vercellini P, Somigliana E, Vigano P, et al. Endometriosis: current and future medical therapies. Best Pract Res Clin Obstet Gynaecol 2008;22:275-306. [Crossref] [PubMed]
- Yap C, Furness S, Farquhar C. Pre and post operative medical therapy for endometriosis surgery. Cochrane Database Syst Rev 2004;2004:CD003678 [PubMed]
- Koshiba A, Mori T, Okimura H, et al. Dienogest therapy during the early stages of recurrence of endometrioma might be an alternative therapeutic option to avoid repeat surgeries. J Obstet Gynaecol Res 2018;44:1970-6. [PubMed]
- Muzii L, Marana R, Caruana P, et al. Postoperative administration of monophasic combined oral contraceptives after laparoscopic treatment of ovarian endometriomas: a prospective, randomized trial. Am J Obstet Gynecol 2000;183:588-92. [Crossref] [PubMed]
- Shaw R, Garry R, McMillan L, et al. A prospective randomized open study comparing goserelin (Zoladex) plus surgery and surgery alone in the management of ovarian endometriomas. Gynaecol Endosc 2001;10:151-7. [Crossref]
- Acién P, Quereda F, Campos A, et al. Use of intraperitoneal interferon alpha-2b therapy after conservative surgery for endometriosis and postoperative medical treatment with depot gonadotropin-releasing hormone analog: a randomized clinical trial. Fertil Steril 2002;78:705-11. [Crossref] [PubMed]
- Loverro G, Carriero C, Rossi AC, et al. A randomized study comparing triptorelin or expectant management following conservative laparoscopic surgery for symptomatic stage III-IV endometriosis. Eur J Obstet Gynecol Reprod Biol 2008;136:194-8. [Crossref] [PubMed]
- Sesti F, Capozzolo T, Pietropolli A, et al. Recurrence rate of endometrioma after laparoscopic cystectomy: a comparative randomized trial between post-operative hormonal suppression treatment or dietary therapy vs. placebo. Eur J Obstet Gynecol Reprod Biol 2009;147:72-7. [Crossref] [PubMed]
- Seracchioli R, Mabrouk M, Frasca C, et al. Long-term cyclic and continuous oral contraceptive therapy and endometrioma recurrence: a randomized controlled trial. Fertil Steril 2010;93:52-6. [Crossref] [PubMed]
- Alborzi S, Hamedi B, Omidvar A, et al. A comparison of the effect of short-term aromatase inhibitor (letrozole) and GnRH agonist (triptorelin) versus case control on pregnancy rate and symptom and sign recurrence after laparoscopic treatment of endometriosis. Arch Gynecol Obstet 2011;284:105-10. [Crossref] [PubMed]
- Chen YJ, Hsu TF, Huang BS, et al. Postoperative maintenance levonorgestrel-releasing intrauterine system and endometrioma recurrence: a randomized controlled study. Am J Obstet Gynecol 2017;216:582.e1-9. [Crossref] [PubMed]
- Jee BC, Lee JY, Suh CS, et al. Impact of GnRH agonist treatment on recurrence of ovarian endometriomas after conservative laparoscopic surgery. Fertil Steril 2009;91:40-5. [Crossref] [PubMed]
- Takamura M, Koga K, Osuga Y, et al. Post-operative oral contraceptive use reduces the risk of ovarian endometrioma recurrence after laparoscopic excision. Hum Reprod 2009;24:3042-8. [Crossref] [PubMed]
- Lee DY, Bae DS, Yoon BK, et al. Post-operative cyclic oral contraceptive use after gonadotrophin-releasing hormone agonist treatment effectively prevents endometrioma recurrence. Hum Reprod 2010;25:3050-4. [Crossref] [PubMed]
- Cucinella G, Granese R, Calagna G, et al. Oral contraceptives in the prevention of endometrioma recurrence: does the different progestins used make a difference? Arch Gynecol Obstet 2013;288:821-7. [Crossref] [PubMed]
- Yamanaka A, Hada T, Matsumoto T, et al. Effect of dienogest on pain and ovarian endometrioma occurrence after laparoscopic resection of uterosacral ligaments with deep infiltrating endometriosis. Eur J Obstet Gynecol Reprod Biol 2017;216:51-5. [Crossref] [PubMed]
- Zhu S, Zhu Y, Liu Y, et al. Comparison of Outcomes of Different Postoperative Hormone Therapy in the Treatment of Ovarian Endometriosis: A Brief Report. Adv Ther 2018;35:857-63. [Crossref] [PubMed]

丁婷
2014年考入四川大学华西临床医学院,2019年至今继续攻读硕士、博士学位,研究方向为妇科肿瘤。在读期间获多项奖学金及优秀研究生,已在国内外期刊发表论文,并多次进行国际、国内会议口头发言及壁报展示,参研多项课题研究。(更新时间:2022-06-24)
袁嘉玲
2012年毕业于四川大学华西临床医学院临床医学八年制专业,获妇产科学博士学位,毕业后留校从事妇产科临床、教学和科研工作至今。现为四川大学华西第二医院妇产科主治医师,任华西临床医学院本科生导师及住院医师规范化培训导师,在妇产科各种常见病、多发病的诊治及处理方面有丰富的临床经验。在国内外期刊发表论文多篇,参研省部级、市级课题多项。(更新时间:2022-06-24)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: D’Alessandro G, Barra F, Tantari M, Ferrero S. Hormonal treatments for preventing recurrence of endometriomas. Gynecol Pelvic Med 2020;3:20.