Multiple uterine leiomyomas removal by single hole laparoscope without pneumoperitoneum suspension
Introduction
Laparoscopic surgery is widely used in a variety of routine gynecological surgery, with shorten wound healing time and hospital stay, recover quickly, spent less, decrease the occurrence of complications. Although the harm brought by pneumoperitoneum laparoscopic surgery keep decreasing with the improvement of insufflators and surgical instruments (1), it is effective in providing exposure, but a series of adverse reactions of metabolic and haemodynamic alterations are associated with the intraperitoneal insufflation of CO2 pneumoperitoneum still exist. Furthermore, laparoscopy performed with pneumoperitoneum has many limitations when dealing with the resection of large symptomatic leiomyoma. Because the pelvic operation with large leiomyoma is somewhat difficult, the bleeding increasing, and even the larger leiomyoma cannot be completely removed. In additional, the surgical field is not well exposed. Meanwhile, it is necessary to carry out leiomyoma pulverization, which the procedure carries certain risks and may lead to the risk of undiagnosed uterine sarcoma fragment implantation and diffusion (2). At last, pneumoperitoneum laparoscopy is also not suitable for many patients who are obese or with advanced disease, or with previous abdominal surgery (3).
In this case, we described a procedure of single hole laparoscope without pneumoperitoneum suspension for a 41-year-old female patient. The patient had a history of regular menstruation, 14 years old of menarche, cycle 28–30 days, period 4–5 days, medium menstrual volume, no history of dysmenorrhea, no blood clots, G3P2A1. She was diagnosed with multiple uterine leiomyomas, along with uterine leiomyomas have been gradually increasing since 2 years ago by vaginal ultrasound, and menstrual volume increased for 1 year, with the menstrual period extending to 7–10 days along with blood clots, and no surgical contraindications were found. The patient was treated by laparoscopy without pneumoperitoneum. The pathological examination showed uterine leiomyoma. The incision healed well and good recovery, patient was discharged on the third day after operation.
Surgical technique
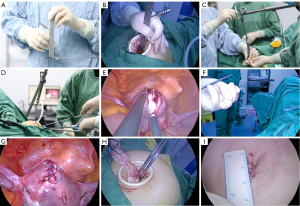
Observation through laparoscope: a little yellow liquid was seen in the rectal fossa, plump uterus, an about 6 cm × 5 cm × 5 cm tumor is prominent in the left anterior wall of the uterus. At the bottom of the uterus, two 1-cm tumor bulges were observed. Both of them smooth surface, clear boundary, activities, medium texture, regular structure. Bilateral fallopian tube and ovaries appear normal. On the right corner, a 2 cm × 2 cm tumor bulge was also found slightly convex, with smooth surface, clear boundary, medium texture and regular structure (preoperative ultrasound suggested that the tumor was convex toward the uterine cavity, and submucosal uterine leiomyomas were considered).
Video 1: multiple uterine leiomyomas removal by single hole laparoscope without pneumoperitoneum suspension.
Surgical procedures: (I) after regular disinfection, unfold the surgical drapes, and implement general anesthesia, then make one about 2-cm long curved incision 0.5 cm alongside the umbilicus toward its superior edge. After cut the skin and subcutaneous tissue, incise and separate muscle by clamping the anterior abdominal fascia, incise into the abdomen after lifting peritoneum. Expand the incision with Yunlong incision protector. Place simple type double leaf retractor in the center of the lower abdomen close to the abdominal wall and open the double leaf retractor to lift the lower abdominal wall, supporting frame with steel draw hook to establish enough space in the abdominopelvic cavity. Finally, place the laparoscope to explore it as depicted above (Figure 1A,B,C,D). (II) Put several stitches in the sigmoid colon mesenteric with 2-0 absorbable suture thread and pull it toward the head to expose the uterus. Inject pituitrin 6 U with saline 10 mL along the myometrium, after uterus contraction and turn white, make a 6-cm longitudinal incision with electrical hook on the left anterior wall along the tumor’s surface. Then lift the tumor with small pliers and dissect tumor pseudocapsule by blunt and sharp dissection with electric hook in order to complete stripping tumors. Suture tumor cavity continuously with size-0 knot-free absorbable suture thread, and continuous suture muscular layer again, finally reinforce and embed muscular layer by suturing. Make a longitudinal incision alongside the fundus to its right uterine horn where the tumor raised, deep into the surface, separate pseudocapsule as above and take out tumors directly via the navel incision. Next expand the incision for about 4 cm, continue to cut muscle layer and lining till the uterine cavity, here the tumor was exposed on the right palace angle, clamp the tumor with small pliers then successfully removed, also taken out directly via the navel incision. Using size-0 knot-free absorbable suture thread continuously suture uterine lining layer, close the uterine cavity, finally continuously suture muscle layer with strengthen the pulp muscular (Figure 1E,F,G). (III) Flush the pelvic cavity to make sure there is no bleeding on each wound, no damage to the pelvic and abdominal organs, and cover the incision on the uterine surface with an absorbable hemostatic gauze. (IV) Small grasping forceps was used to lift the tumor from the left anterior wall to the umbilical incision. The tumor was successfully removed after rotary cutting with a sharp knife and clamped with sharp forceps because of the tumor was too large to be directly removed (Figure 1H). (V) Release the suspension wire, close and take out the double-lobed retractor at the abdominal wall from the abdominal cavity under laparoscopy. Clamp the peritoneum along both sides of the Yunlong incision protector and take out it, then suture the peritoneum continuously with 2-0 absorbable line, the abdominal wall fascia and subcutaneous tissue layer by layer. In the end suture the incision intercutaneous with 3-0 absorbable line, and the operation is complete (Figure 1).
The anesthesia was satisfactory and the operation went smoothly. It took 78 minutes and the amount of bleeding was about 20 mL.
Comments and discussion
For pneumoperitoneum laparoscopy, CO2 gas and its devices were the most commonly used and relied on. During operation CO2 pneumoperitoneum causes intra-abdominal pressure rise and diaphragm elevated, plus pushing pressure from intra-abdominal organs makes thoracic expansion limited, airway resistance increased, lung compliance decreased, patient tidal volume decreased, ventilation/blood flow ratio imbalance, pet CO2 increased, and blood pH decreased (4).
Now CO2 gas is not used in the laparoscopy, which eliminates the complications related to CO2 and expands the indications for surgery. Therefore, Gasless laparoscopy is more suitable for patients who cannot tolerate general anesthesia or with cardiopulmonary dysfunction. And surgery can be performed under epidural anesthesia (5). Without gas laparoscopy requires no gas and no other operator. There is no need for intraoperative and exhalation CO2 monitor and related instruments, also special single-hole instrument and operating platform. The no pneumoperitoneum suspension instrument can be used repeatedly, which is more economical than the expensive disposable puncture needle and single-hole operating platform. The equipment can be assembled at a tenth of the cost of pneumoperitoneum equipment and used for a long time.
Gasless laparoscopy also widely applied to the field of routine gynecological surgery like pneumoperitoneum, without the influence of CO2. Furthermore, laparoscopic surgery without pneumoperitoneum can reduce the size of a large uterine leiomyoma directly at the umbilical incision, It has more advantages in the treatment for patient who cannot tolerate pneumoperitoneum or with cardiopulmonary dysfunction.
To further improve the effect of the surgery, we develop and innovate to change the current double-leaf retractor to three-leaf one, which is currently in the process of patenting. Then replace retractor at the center of the lower abdomen with sustainable smoke extractor to improve operating clarity, the extra space is convenient for continuous stable operation and avoid affecting the normal. The no-pneumoperitoneum suspension device currently we use has the advantages of simple install and operate. During the operation the device can move freely in and out the abdominal cavity without being affected by pneumoperitoneum, also suture is more simply. The suture needle and the suture thread can get through the navel incision every time. The suture thread can be intensified outside the abdominal cavity, and reenter the abdominal cavity for suture after holding the needle, so as to solve the problem of knotting in the abdominal cavity when the suture line is long (6). Furthermore, it is easier to remove the specimens directly from the umbilical incision. Without the influence of the pneumoperitoneum, continuous aspiration of smoke can maintain clear vision. For gynecological gasless laparoscopic suspension surgery, we should not only understand its advantages, but also understand its limitations, so as to objectively and scientifically evaluate its supplement value of conventional laparoscopic surgery, for example, because there is no carbon dioxide to insufflate abdominal push up effect during gasless laparoscopic surgery, so the intraoperative for upper abdomen revealed is poorer, the need to further improve in the future.
In conclusion, gasless laparoscopic surgery is more appropriate applies to patient who cannot tolerate pneumoperitoneum or with cardiopulmonary dysfunction. Conventional laparoscopic instruments can be used. Compared with pneumoperitoneum laparoscopy surgery, there is no need to apply traditional pneumoperitoneum equipment and use disposable operating platform consumables to reduce the economic burden of patients. Currently, 40 cases of no pneumoperitoneum single-arch laparoscopic surgery have been performed in our hospital. It includes hysterectomy, ectopic pregnancy, ovarian cyst, infertility, caesarean section, uterine leiomyoma and so on. It is worth promoting on account of simple no prolonged operative time, no increased intraoperative blood loss with no special equipment and consumables applied. For no pneumoperitoneum suspension laparoscopy, we should understand its advantages over traditional laparoscopy, and also fully understand its limitations. In this way, we can objectively and scientifically evaluate its complementary value as routine (pneumoperitoneum) laparoscopic surgery, and then exert its unique advantages, such as eliminating or relieving pneumoperitoneum complications.
Acknowledgments
The video was awarded the second prize in the Second International Elite Gynecologic Surgery Competition (2020 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Second International Elite Gynecologic Surgery Competition (2020 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Peer Review File: Available at https://gpm.amegroups.org/article/view/10.21037/gpm-20-72/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-20-72/coif). The series “Award-Winning Videos from the Second International Elite Gynecologic Surgery Competition (2020 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bickel A, Arzomanov T, Ivry S, et al. Reversal of adverse hemodynamic effects of pneumoperitoneum by pressure equilibration. Arch Surg 2004;139:1320-5. [Crossref] [PubMed]
- Mathevet P, Nessah K, Dargent D, et al. Laparoscopic management of adnexal masses in pregnancy: a case series. Eur J Obstet Gynecol Reprod Biol 2003;108:217-22. [Crossref] [PubMed]
- Chang FH, Soong YK, Cheng PJ, et al. Laparoscopic myomectomy of large symptomatic leiomyoma using airlift gasless laparoscopy: a preliminary report. Hum Reprod 1996;11:1427-32. [Crossref] [PubMed]
- Schwarte LA, Scheeren TW, Lorenz C, et al. Moderate increase in intraabdominal pressure attenuates gastric mucosal oxygen saturation in patients undergoing laparoscopy. Anesthesiology 2004;100:1081-7. [Crossref] [PubMed]
- Jansen FW, Kapiteyn K, Trimbos-Kemper T, et al. Complications of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol 1997;104:595-600. [Crossref] [PubMed]
- Koo YJ, Song HS, Im KS, et al. Multimedia article. Highly effective method for myoma excision and suturing in laparoscopic myomectomy. Surg Endosc 2011;25:2362. [Crossref] [PubMed]
Cite this article as: Sun C, Mao X, Lin M, Liu Y, Ding X, Zhang X. Multiple uterine leiomyomas removal by single hole laparoscope without pneumoperitoneum suspension. Gynecol Pelvic Med 2021;4:27.