The #Enzian classification for the diagnosis and surgery of endometriosis: a narrative review
Introduction
Endometriosis is a highly complex disease with a variety of clinical presentations and symptoms. To streamline diagnosis and therapy, to assess treatment outcome, and to permit research, the severity and presentation of this disease need a classification.
A meaningful classification of endometriosis must, on the one hand, comprehensibly represent the entire extent and nature of endometriosis and, on the other hand, take into account the requirements for predictive value, or allow estimation of the outcome.
Given the many uncertainties in the pathophysiology of endometriosis, classification today is limited to clinical observations that can be used to predict an outcome. The current classifications thus are based on observations during surgery.
After the era of microsurgery using laparotomy, surgical treatment of endometriosis was mainly carried out by laparoscopy. In the last decades, the development of new instruments such as lasers, sealing instruments and 3D cameras, and other devices have improved and differentiated the surgical treatment of endometriosis. Also, imaging by transvaginal sonography (TVS) and magnetic resonance imaging (MRI) has improved and permitted a differentiated diagnosis with MRI examinations and high-resolution ultrasound.
A common classification system is important to assess the diagnostic accuracy and predictive value of imaging and to evaluate the value of preoperative imaging in helping or improving surgery, which can be unexpectedly difficult and which is complication prone.
Several studies demonstrated the accuracy of sonographic diagnosis when compared with surgical findings.
The problem of the inadequate classification of endometriosis will be addressed on the basis of the available data in the literature. The further developed system of the Enzian classification, the #Enzian classification, as a comprehensive system, is presented and analyzed (1).
The selection and analysis of the most frequently cited publications on the classifications was done by PK, GH and JK, taking into account the clinical relevance.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-38/rc).
Classification systems for endometriosis
The Acosta classification (2) distinguished superficial endometriosis and small and large ovarian endometriosis. The addition of a point scoring system for a pelvic area of superficial endometriosis and the severity, size, and bilaterality of cystic ovarian endometriosis and the associated adhesions led to the American Fertility Society (AFS) classification system, published in 1979 (3), and became widely used. Revisions were made in 1985 and 1996 (4), the last one is now used as the revised American Society for Reproductive Medicine (rASRM) classification (5).
To understand the rASRM classification, we need to realize that it was developed by reproductive surgeons when surgery for cystic ovarian endometriosis was still mainly done by microsurgery with initial attempts to destroy typical endometriosis lesion by laparoscopy. Subtle lesions had not yet been recognized as endometriosis (6) and it would take 10 years before the importance of deep endometriosis (DE) was realized (7). It thus is not surprising that neither subtle nor DE lesions were represented in the AFS classification (Figure 1). Also the problem of the severe pain symptoms, and the dysfunction because of involvement of adjacent organs such as bowel, bladder, and ureter, and the difficulty of surgery and postoperative adhesion formation, were not considered. That is why the rASRM classification poorly correlates with the severity of pelvic pain, and that most DE lesions are found in women classified as rASRM II and rASRM III (8). Also in our study in 63 patients with DE including recto-sigmoid endometriosis, 21% were found to have only stage 1 or 2 according to the rASRM scoring system (9).
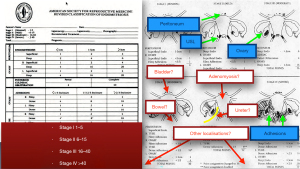
Figure 1: illustration of the rASRM classification. Using a very differentiated scoring system, four stages are determined (stage I–IV). All endometriosis lesions in the pelvis at the peritoneum, ovary and utero sacral ligament (USL) (all marked in blue) as well as adhesions are taken into account. Extra pelvic endometriosis as well the various localizations of DE (marked in red) are classified incompletely, but mostly not at all. Few studies attempted to evaluate the usefulness of the rASRM classification for TVS or MRI imaging. These studies moreover are biased, since the accuracy of imaging is very good for ovarian endometriosis but poor for superficial small endometriosis lesions. The accuracy of TVS- or MRI-based staging of endometriosis using the rASRM score has not been evaluated in large studies. In small studies, Leonardi et al. (10) compared the diagnostic accuracy of TVS with surgical rASRM classification in a retrospective study. The overall accuracy was only 53.4% for rASRM stage 1, but 93.1% for stage 4, confirming the accuracy of imaging for cystic ovarian endometriosis. Similarly, Williams et al. (11) showed in 65 patients that kissing and retro positioned ovaries diagnosed by MRI were associated with higher intraoperative rASRM stages.
The first validation of a classification system of endometriosis is whether it predicts pelvic pain, infertility, or difficulty of surgery (12). The rASRM classification does poorly predict any of these as demonstrated by Vercellini et al. (13) and Fedele et al. (14). The association between rASRM stages and the degree and type of pelvic symptoms was inconsistent. This is not surprising to know the absence of DE in the rASRM classification, while DE is more frequent than anticipated previously and causes severe pain (15). This was confirmed by Chapron et al. (16) showing a correlation between the severity of dysmenorrhea and the presence of posterior DE, but no correlation between rASRM and pain or postoperative pregnancy rates (17). Similar inconsistent results were found when rASRM stages were correlated with operative difficulty and complications (18). Also, Poupon, using a nomogram, couldn’t observe a correlation between rASRM stages and the occurrence of complications (19).
The second type of validation of a classification system is the accuracy and reliability of registration. As expected, a web-based dynamic registration and scoring system for endometriosis (E-QUSUM), improves the accuracy of registration by permitting more information and help. This was demonstrated for rASRM, Enzian, and EFI scores. It moreover is more user-friendly. In a study of 40 endometriosis specialists, Metzemaekers et al. (20) compared the scoring using the common “paper form” questionnaires with using a computer recording program (EQUSUM) (20). The complex system of rASRM classification with its various exceptions proved to be error-prone unless used digitally even if used by experts. None of them succeeded to properly classify all pre-defined cases with rASRM in paper form, although 70% were classified correctly electronically. The Enzian classification was 70% correct on paper, but 90% by EQUSUM, demonstrating indirectly the reliability of scoring with Enzian classification.
In conclusion, although the rASRM classification is the most commonly used, it is a complex and error-prone paper form. It is inappropriate for DE and poorly predicts pain or infertility or surgical difficulty or outcome.
Therefore an alternative or additional classification system, including DE is needed as often debated (21,22).
Enzian classification
The Enzian classification was created in 2003 (23) as a detailed description of the location and size or severity of DE lesions. If used in combination with the rASRM classification, superficial and ovarian endometriosis are scored. It can be used also for TVS and MRI imaging of DE (24-27) and the imaging results correlate with the surgical observations as recently demonstrated by Hudelist et al. (28).
The Enzian scoring system was validated by demonstrating a correlation between the localization of DE and the symptoms (26). Haas et al. demonstrated that the Enzian classification correlates with the duration and the difficulty of surgery (29) and that some postoperative complications correlate with specific locations.
Roman and colleagues (30) compared the outcome of three different surgical approaches to rectal endometriosis with the size of the lesions according to the Enzian classification (size of rectal lesion: <1, 1–3, and >3 cm). Based on the correlation between duration of surgery, complication rate, and size of the lesion according (Enzian score) recommendations were made.
Poupon et al. compared the risk of surgical complications with the Enzian classification, taking into account and in addition patient age and previous surgeries for endometriosis (19). A significant increase of severe grade III complications was observed in a high-risk group with at least A3, B3, or C1 location (OR =3.918; 95% CI: 1.229–12.484). No such correlation was observed regarding complication rates between rASRM stages I and II or between ASRM stages III and IV. A similar finding is described by Nicolaus (18).
Imboden et al. (31) demonstrated a significant association between the presence of Enzian B lesions and the incidence of postoperative severe bladder voiding dysfunction.
The possibility of being able to carry out the classification non-invasively, to analyze symptoms and predict the surgical difficulties opens new aspects in the treatment of endometriosis, which was not demonstrated using the ASRM classification (18).
Thus, it is not surprising that this can be substantially helpful for counseling the patient and planning a surgical intervention as well as for interdisciplinary help.
The endometriosis fertility index (EFI)
The EFI (Figure 2) published in 2010 by Adamson et al. (32) is estimates the probability of conception in women with endometriosis and infertility. The EFI combines in a 10-point scoring system all known predictive factors such as patient age, duration of infertility and previous pregnancies, and the rASRM classification and postoperative tubo-ovarian function. The latter combines an evaluation of the fallopian tubes, tubal fimbriae, and ovaries (Figure 2).
Of the 10 points assessment, only two points are directly related to endometriosis. The adnexal function is important, but the potential endometriosis involvement is not taken into account. Its clinical applicability and value have been confirmed (33) and EFI has gained wide acceptance among reproductive surgeons involved in MAR (34,35). However, EFI is not a classification for endometriosis.
The future
The Enzian classification is the only clinical classification of DE. It is widely used in German-speaking countries and is adopted by several other international and national societies. The predictive clinical value of Enzian classification has already been studied in terms of duration of surgery and complication rate but needs further detailed studies in terms of prognosis of the disease. Large series will be necessary to compensate for the complexity of the disease, for the skills of the surgeon, and important outcome factors as rare complications. This contrasts with the rASRM classification for which we know it has no predictive value for the surgical outcome, which is not surprising since DE is not reflected in that classification.
Enzian has the potential advantage of permitting the combination of non-invasive and invasive procedures. Preliminary data demonstrate a strong correlation of preoperative Enzian classification by imaging and perioperative Enzian classification. This highlights the potential of predicting the outcome of surgery by preoperative imaging. This might permit to demonstrate that preoperative imaging can guide the surgeon, eventually, to excise lesions that otherwise would remain undetected. Whether imaging can help in avoiding a diagnostic laparoscopy, in women with minimal symptoms is another discussion (36).
The Enzian classification was recently updated to the #Enzian classification to become a comprehensive classification by including superficial and cystic ovarian endometriosis (37).
The #Enzian classification is designed to comprehensively evaluate all types, localizations, and sizes of endometriosis, together with the involvement of other organs and eventual other localizations. The Enzian classification is a purely descriptive surgical classification without preset assumptions or simplifications, thus permitting statistical analysis.
Since the #Enzian classification moreover permits to be used for preoperative imaging, it is a unifying language for specialties ranging from sonographers and radiologists to surgeons (37,38).
The significant accurate matching of preoperative sonographic findings to those at surgery, using #Enzian classification, was demonstrated by Di Giovanni in a retrospective study of 93 women. This study took place in a high level tertiary center for endometriosis (39). Very similar results were obtained in a recently completed prospective multicenter study of 745 patients classified by both TVS and surgery (37).
The #Enzian classification
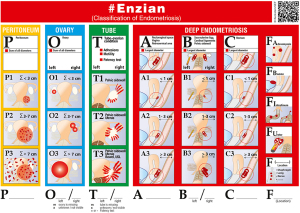
The #Enzian classification (Figure 3) is a descriptive classification without predefined classes and assumptions thus permitting statistical validation as described previously (37). The location and severity of superficial, cystic ovarian, and DE and the involvement of other organs are registered using pictograms facilitating scoring (Figure 3). Location and type are described by a letter. Superficial endometriosis is indicated by P (peritoneum), ovarian by O (ovary), DE of the anterior, lateral, and posterior compartments by A, B, and C, respectively. The adnexal adhesions, including the tubal patency, are indicated by T and the involvement of other organs by F, i.e., FA for Adenomyosis, FI for other bowel involvement, FB for bladder involvement, FU for ureter involvement, and the individual measurements were taken into account in one dimension, and the direction of the measurement is shown in Figure 3.
Coding
Thus, the location of endometriosis lesions is described by a code as follows: #Enzian P_, O_/_, T _/_, A _, B_/_, C _, F_ (localization).
The severity or extend of endometriosis is graded as 1, 2 or 3, which is a simplification permitting pictograms instead of registering diameters and surface areas. For organs occurring bilaterally, as the ovary, tube, USL, parametrium, and ureter location are indicated after the capital letter and separated by a slash.
The peritoneal (P) area covered by superficial endometriosis was scored as less (P1) or more (P2) than 3 cm in diameter. This corresponds in over 95% to the revised AFS (rAFS) classes I and II (8). A class P3 was added for areas more than 7 cm, to account for those patients with very extensive endometriosis. When assessing the “P stage”, the diameter of a virtual circle is calculated in which all endometrial foci can be included. P1 =<3 cm (sum of all lesions), P2 =3–7 cm (sum of all lesions), P3 =>7 cm (sum of all lesions).
Ovarian (O) endometriosis was scored as O1 if less than 3 cm in diameter since the ESHRE classification arbitrarily suggested that for cysts less than 3 cm surgery could be avoided. A diameter of 3–7 cm was used to select a stage O2, which is more likely to be operated, and a diameter of more than 7 cm stage O3 was used. With this size, great damage to the ovary itself is to be expected, but also a significantly increased risk with a possible surgical therapy with regard to ovarian function. All endometriomas and infiltrating ovarian surface foci (≥5 mm) are considered as ovarian endometriosis. In case of multilocular endometriomas, sums of the maximal diameter of all lesions are separately calculated for each side.
Example for evaluating the ovaries: left ovary, the diameter of the endometrioma 1 cm corresponds to O1; right ovary 8 cm corresponds to O3, the coding is then #Enzian O1/3. Missing organs are described with suffix m. Non visualized organs by x.
Peritubal and periadnexal adhesions (T) are classified as reflects T1 for adhesions of the adnexa to the pelvic wall, as T2 for adhesions between the adnexa pelvic wall and uterus, and as T3 for additional adhesions to the bowel. A similar classification is used for TVS using soft markers as sliding signs (40).
DE (A, B, C, F): the Enzian classification is based on different compartments where each localization/organ is taken into account. These are represented by the compartments A [craniocaudal axis = vagina, rectovaginal space (RVS), retro cervical space, torus], B (mediolateral axis = USLs, cardinal ligaments, pelvic sidewall) and C (ventrodorsal axis = rectum).
DE in the uterus and other extragenital locations (F): adenomyosis (FA), bladder involvement (FB), extrinsic and/or intrinsic ureteric involvement with signs of obstruction (FU), bowel disease (FI) cranial to the rectosigmoid junction (>16 cm from the anal verge; upper sigmoid, transverse colon, caecum, appendix, small bowel) and other locations (FO) such as the abdominal wall, diaphragm, and nerve.
For the sonographic description, the recommendations of systematic evaluation of International Deep Endometriosis Analysis Group (IDEA) (40) are used to describe findings of localization and size accurately. The individual measurements were taken into account in one dimension, and the direction of the measurement is shown in Figure 3.
How to use #Enzian classification: example
The differentiated use of the #Enzian classification is demonstrated using the following example (Figures 4-8).
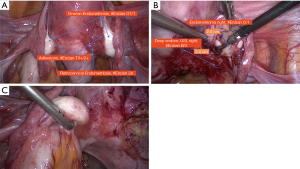
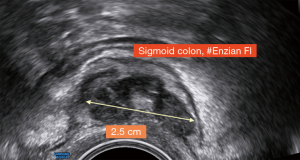

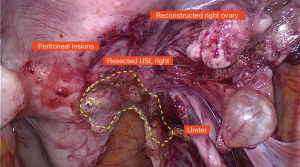

Findings: visible lesions on the peritoneum, ovaries left/right, USL left/right, and sigmoid colon, adhesions on both ovaries to pelvic sidewall and uterus.
The example shows that diagnostic laparoscopy is not always sufficient to fully classify endometriosis. Both the extent of intramural bowel endometriosis and the localization and extent of e.g., deep-seated adenomyosis often only become fully visible when the organ structures are completely exposed or and the pathology is removed in toto. It is obvious that preoperative sonography or MRI greatly facilitates the identification and assessment of these structures.
The findings (Figures 4-8) are classified or documented in (Table 1) a code.
Table 1
| Localisation and extent of the different lesions | Code |
|---|---|
| Superficial endometriosis on the peritoneum 3–7 cm (P) | = P2 |
| Ovarian endometriosis, left 0.5 cm/right 2 cm (O) | = O1/1 |
| Adhesions between tubo-ovarian unit to pelvic side wall and uterus (right) and to the bowel (left) (T) both tubes patent | = T3+/2+ |
| DE, left USL 1.2 cm, right USL 2.5 cm (B) | = B2/2 |
| DE on sigmoid colon (FI) | = FI |
| #Enzian(s) P2, O1/2, T3+/2+, B2/2, FI | |
| Final coding with #Enzian classification, merging both, the laparoscopic (Figures 4,6,7) and ultrasound findings (Figures 5,8) | |
| DE on sigmoid colon (nodule 2.6 cm) | = FI (sigmoid) |
| Uterus (adenomyosis) | = FA |
| #Enzian(s,u) P2, O1/2, T3+/2+, B2/2, FI(u) FA(u) |
The findings (Figures 4-8) are summarized in detail in this table. Primarily, the classification here was made by laparoscopy (Figures 4,6,7), which is indicated by the suffix(s). The additional findings identified with TVS(u) (Figures 5,8) are combined in one code [#Enzian(s,u)]. This enables a complete recording of all findings. The disadvantage that each method does not clearly detect all foci is thus significantly improved. USL, utero sacral ligament; DE, deep endometriosis.
Discussion
Classification of the disease has been used primarily for the postoperative staging of the disease. Unfortunately, the most commonly used rASRM classification does not correlate with symptoms or other important parameters, and cannot be used for non-invasive diagnostics. Moreover, it does not take into account DE but also extra pelvic endometriosis.
The EFI is valid for calculating the probability of pregnancy in a patient with endometriosis.
It does not contain any detailed information on the location and extent of lesions, especially DE.
The Enzian classification is predominantly used to describe DE.
The #Enzian classification is a descriptive and complete classification of endometriosis, taking into account that the size of the lesions matters and that involvement of other organs determine the surgical difficulty and also risk. It thus will permit validation since the predictive value of type, localization, and extent of each type of lesion can be calculated for each outcome parameter as pain relief, fertility, and complication of surgery.
However, it should be understood that similar to diagnostic tests, the clinician needs to know the predictive value or a scoring. This is very different from statistically significant correlations and differences. Although men are significantly taller than women, height is a poor predictor of sex.
The #Enzian score is a smart simplification of an ideal scoring system based on pictograms, to improve user-friendliness and reliability of registration. It is a simplification since predefined classes are used instead of actual diameters. The latter would have made it possible to assess which classes should be used. However, the decisions made have the advantage of allowing pictograms, while the decisions made are based on a solid evidence The superficial peritoneal classes 1 and 2 correspond to the rASRM classes I and II in over 95% (8). The 3 classes of ovarian endometriosis correspond to lesions that might not be operated on (less than 3 cm), which are an indication for surgery (3 to 7 cm), and those which risk causing so much ovarian damage that a two-step surgery is advocated (>7 cm) (41). The classes of DE are based on the common knowledge that surgery becomes exponentially more difficult for larger lesions. However, the exact assessment of the size of the DE is also subject to a partly subjective assessment by the surgeon. This is very much influenced by the location, the type of endometriosis, the accompanying tissue reactions and also the type of surgical access, which can possibly lead to a certain inaccuracy. This imprecision of detection was taken into account by selecting only three classes. It is a smart simplification when considering what is not registered. Although debated, subtle lesions are not classified separately since also rASRM does not. It seems reasonable to separate peri adnexal adhesions from ovarian endometriosis as it balances ease of use and completeness. Validation would require a large number of observations due to the variability of endometriosis.
The diagnosis and treatment of endometriosis have changed over the last decade by progress in surgery, and imaging. A major advantage of #Enzian classification is that it bridges the gap between imaging and surgery since they can use the same classification.
Preoperative classification by imaging (MRI and TVS) has the added advantage that it could be useful for predicting the difficulty and duration of surgery. Measurement by imaging is likely to be more accurate. This contrasts with surgical classification by measuring the surgical field, the surgical specimen or the assessment of the specimen by the pathologist. The accuracy of measuring or estimating the extent of the disease is a crucial question. #Enzian wants to solve this through a compromise between accuracy and feasibility. Compared to the ASRM classification, a much better representation of the disease has become possible (39,42).
Through the detailed coding of the individual findings, the extent of the findings can be completely mapped. The idea of using suffixes to additionally indicate the type of findings serves a multidisciplinary approach. Some findings are difficult to identify surgically. To perform a complete surgical staging would even require an unnecessary extension of the procedure in patients with minimal symptoms.
Its application also allows to classify findings in MRI and TVS and to assess the difficulty of the surgical procedure and the risk of complications in surgical procedures. The different imponderables in diagnosis remain a very important and interesting field for future research, and whether the #Enzian can be used to predict fertility outcomes remains to be determined.
Conclusions
The #Enzian classification represents a comprehensive description of peritoneal and ovarian endometriosis as well as adnexal adhesions in addition to DE.
#Enzian provides a classification system that is anatomically logical, easy to use, and reproducible for the complete description of endometriosis. The correlation between preoperative and surgical staging, based on the #Enzian scheme allows for consistent and clear classification of endometriosis, especially DE but also secondary adhesions. Endometriosis can be mapped completely with one single classification system applicable by pre-invasive and invasive methods thereby enabling the use of one common language for describing endometriosis. The detailed description of the disease enables better care of the patient concerning symptoms, clinical findings, and therapy as well as scientific studies.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Andrea Tinelli) for the series “Endometriosis Surgery” published in Gynecology and Pelvic Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-38/rc
Peer Review File: Available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-38/coif). The series “Endometriosis Surgery” was commissioned by the editorial office without any funding or sponsorship. PK serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from December 2020 to November 2022. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abrao MS, Gonçalves MO, Dias JA Jr, et al. Comparison between clinical examination, transvaginal sonography and magnetic resonance imaging for the diagnosis of deep endometriosis. Hum Reprod 2007;22:3092-7. [Crossref] [PubMed]
- Acosta AA, Buttram VC Jr, Besch PK, et al. A proposed classification of pelvic endometriosis. Obstet Gynecol 1973;42:19-25. [PubMed]
- Classification of endometriosis. The American Fertility Society. Fertil Steril 1979;32:633-4. [Crossref] [PubMed]
- Johnson NP, Hummelshoj L, Adamson GD, et al. World Endometriosis Society consensus on the classification of endometriosis. Hum Reprod 2017;32:315-24. [Crossref] [PubMed]
- Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril 1997;67:817-21. [Crossref] [PubMed]
- Jansen RP, Russell P. Nonpigmented endometriosis: clinical, laparoscopic, and pathologic definition. Am J Obstet Gynecol 1986;155:1154-9. [Crossref] [PubMed]
- Cornillie FJ, Oosterlynck D, Lauweryns JM, et al. Deeply infiltrating pelvic endometriosis: histology and clinical significance. Fertil Steril 1990;53:978-83. [Crossref] [PubMed]
- Koninckx PR, Meuleman C, Demeyere S, et al. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril 1991;55:759-65. [Crossref] [PubMed]
- Wustlich M. Laparoscopic assited segmental resection in endometriosis with bowel involvement (Laparoskopisch-assistierte Sigmasegmentresektionbei Endometriose mit Darmbeteiligung). Ulm: University Ulm, 2002.
- Leonardi M, Espada M, Choi S, et al. Transvaginal Ultrasound Can Accurately Predict the American Society of Reproductive Medicine Stage of Endometriosis Assigned at Laparoscopy. J Minim Invasive Gynecol 2020;27:1581-7.e1. [Crossref] [PubMed]
- Williams JC, Burnett TL, Jones T, et al. Association between kissing and retropositioned ovaries and severity of endometriosis: MR imaging evaluation. Abdom Radiol (NY) 2020;45:1637-44. [Crossref] [PubMed]
- Koninckx PR, Ussia A, Adamyan L, et al. An endometriosis classification, designed to be validated. Gynecol Surg 2011;8:1-6. [Crossref]
- Vercellini P, Fedele L, Aimi G, et al. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod 2007;22:266-71. [Crossref] [PubMed]
- Fedele L, Bianchi S, Bocciolone L, et al. Pain symptoms associated with endometriosis. Obstet Gynecol 1992;79:767-9. [PubMed]
- Andres MP, Borrelli GM, Abrão MS. Endometriosis classification according to pain symptoms: can the ASRM classification be improved? Best Pract Res Clin Obstet Gynaecol 2018;51:111-8. [Crossref] [PubMed]
- Chapron C, Fauconnier A, Dubuisson JB, et al. Deep infiltrating endometriosis: relation between severity of dysmenorrhoea and extent of disease. Hum Reprod 2003;18:760-6. [Crossref] [PubMed]
- Vercellini P, Fedele L, Aimi G, et al. Reproductive performance, pain recurrence and disease relapse after conservative surgical treatment for endometriosis: the predictive value of the current classification system. Hum Reprod 2006;21:2679-85. [Crossref] [PubMed]
- Nicolaus K, Zschauer S, Bräuer D, et al. Extensive endometriosis surgery: rASRM and Enzian score independently relate to post-operative complication grade. Arch Gynecol Obstet 2020;301:699-706. [Crossref] [PubMed]
- Poupon C, Owen C, Arfi A, et al. Nomogram predicting the likelihood of complications after surgery for deep endometriosis without bowel involvement. Eur J Obstet Gynecol Reprod Biol X 2019;3:100028. [Crossref] [PubMed]
- Metzemaekers J, Haazebroek P, Smeets MJGH, et al. EQUSUM: Endometriosis QUality and grading instrument for SUrgical performance: proof of concept study for automatic digital registration and classification scoring for r-ASRM, EFI and Enzian. Hum Reprod Open 2020;2020:hoaa053.
- Abrao MS, Neme RM, Carvalho FM, et al. Histological classification of endometriosis as a predictor of response to treatment. Int J Gynaecol Obstet 2003;82:31-40. [Crossref] [PubMed]
- Adamson GD. Endometriosis classification: an update. Curr Opin Obstet Gynecol 2011;23:213-20. [Crossref] [PubMed]
- Keckstein J, Ulrich U, Possover M, et al. ENZIAN-Klassifikation der tief infiltrierenden Endometriose. Zentralbl Gynäkol 2003;125:291.
- Di Paola V, Manfredi R, Castelli F, et al. Detection and localization of deep endometriosis by means of MRI and correlation with the ENZIAN score. Eur J Radiol 2015;84:568-74. [Crossref] [PubMed]
- Burla L, Scheiner D, Hötker AM, et al. Structured manual for MRI assessment of deep infiltrating endometriosis using the ENZIAN classification. Arch Gynecol Obstet 2021;303:751-7. [Crossref] [PubMed]
- Montanari E, Dauser B, Keckstein J, et al. Association between disease extent and pain symptoms in patients with deep infiltrating endometriosis. Reprod Biomed Online 2019;39:845-51. [Crossref] [PubMed]
- Thomassin-Naggara I, Lamrabet S, Crestani A, et al. Magnetic resonance imaging classification of deep pelvic endometriosis: description and impact on surgical management. Hum Reprod 2020;35:1589-600. [Crossref] [PubMed]
- Hudelist G, Montanari E, Salama M, et al. Comparison between Sonography-based and Surgical Extent of Deep Endometriosis Using the Enzian Classification - A Prospective Diagnostic Accuracy Study. J Minim Invasive Gynecol 2021;28:1643-9.e1. [Crossref] [PubMed]
- Haas D, Chvatal R, Habelsberger A, et al. Preoperative planning of surgery for deeply infiltrating endometriosis using the ENZIAN classification. Eur J Obstet Gynecol Reprod Biol 2013;166:99-103. [Crossref] [PubMed]
- Roman H, Moatassim-Drissa S, Marty N, et al. Rectal shaving for deep endometriosis infiltrating the rectum: a 5-year continuous retrospective series. Fertil Steril 2016;106:1438-45.e2. [Crossref] [PubMed]
- Imboden S, Bollinger Y, Härmä K, et al. Predictive Factors for Voiding Dysfunction after Surgery for Deep Infiltrating Endometriosis. J Minim Invasive Gynecol 2021;28:1544-51. [Crossref] [PubMed]
- Adamson GD, Pasta DJ. Endometriosis fertility index: the new, validated endometriosis staging system. Fertil Steril 2010;94:1609-15. [Crossref] [PubMed]
- Garavaglia E, Pagliardini L, Tandoi I, et al. External validation of the endometriosis fertility index (EFI) for predicting spontaneous pregnancy after surgery: further considerations on its validity. Gynecol Obstet Invest 2015;79:113-8. [Crossref] [PubMed]
- Tomassetti C, Bafort C, Vanhie A, et al. Estimation of the Endometriosis Fertility Index prior to operative laparoscopy. Hum Reprod 2021;36:636-46. [Crossref] [PubMed]
- Tomassetti C, Geysenbergh B, Meuleman C, et al. External validation of the endometriosis fertility index (EFI) staging system for predicting non-ART pregnancy after endometriosis surgery. Hum Reprod 2013;28:1280-8. [Crossref] [PubMed]
- Goncalves MO, Siufi Neto J, Andres MP, et al. Systematic evaluation of endometriosis by transvaginal ultrasound can accurately replace diagnostic laparoscopy, mainly for deep and ovarian endometriosis. Hum Reprod 2021;36:1492-500. [Crossref] [PubMed]
- Keckstein J, Saridogan E, Ulrich UA, et al. The #Enzian classification: A comprehensive non-invasive and surgical description system for endometriosis. Acta Obstet Gynecol Scand 2021;100:1165-75. [Crossref] [PubMed]
- Keckstein J, Hudelist G. Classification of deep endometriosis (DE) including bowel endometriosis: From r-ASRM to #Enzian-classification. Best Pract Res Clin Obstet Gynaecol 2021;71:27-37. [Crossref] [PubMed]
- Di Giovanni A, Montanari E, Hudelist G, et al. Comparison between sonography-based and surgical evaluation of endometriotic lesions using the #Enzian classification – a retrospective data analysis. European Journal of Ultrasound 2021; In press.
- Guerriero S, Condous G, van den Bosch T, et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet Gynecol 2016;48:318-32. [Crossref] [PubMed]
- Working group of ESGE. Recommendations for the surgical treatment of endometriosis-part 1: ovarian endometrioma. Gynecol Surg 2017;14:27. [Crossref] [PubMed]
- Montanari E, Bokor A, Szabó G, et al. Accuracy of sonography for non-invasive detection of endometriosis using the #Enzian classification – a prospective multicentre diagnostic accuracy study. Ultrasound in Obstetrics & Gynecology 2021; In press.
Cite this article as: Keckstein J, Hudelist G, Koninckx P, Keckstein S, Keckstein S. The #Enzian classification for the diagnosis and surgery of endometriosis: a narrative review. Gynecol Pelvic Med 2021;4:40.