Tubal pregnancy complicated with rudimentary horn: two case reports and literature review
Introduction
The incidence of müllerian duct anomalies has been estimated in 0.16–10% of all women and unicornuate uterus accounts for 4–5% of these cases (1-3), although the true incidence is unknown. Although tubal pregnancy is the most common ectopic pregnancy, tubal pregnancy in a unicornuate uterus with rudimentary horn has rarely been documented. Here we present the clinical manifestations and management of two cases of tubal pregnancy in a unicornuate uterus with rudimentary horn and reviewed the literature on this topic. We present the following cases in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-43/rc).
Case presentation
This study was approved by the Institutional Review Board of West China Second University Hospital of Sichuan University [Approval No. 006(2020)]. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Case 1
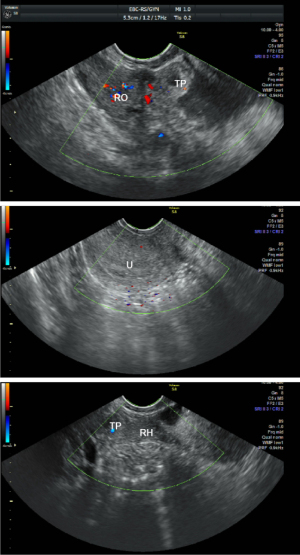
A 32-year-old female, G1P0, presented with amenorrhea for 45 days’ duration with lower abdominal pain. She experienced no vaginal bleeding during this period. This patient’s menarche was at 13 years and she had regular menstrual cycles and mild dysmenorrhea. Past medical and social histories were unremarkable. Physical examination: cervix, no lifting pain; uterus, anterior position, normal size, no pressure pain; right adnexal area, a mass of about 5-cm-diameter was detected, movable, mild tenderness; left adnexal area, no abnormality. Her blood showed β-human chorionic gonadotrophin (β-HCG) at 5,742 mIU/mL. Transvaginal ultrasonography revealed no gestational sac in the uterus, of which right cornu was not clear. A 3.3×1.4×1.7 cm hypoechoic mass connecting to the right anterior wall of the uterus was observed in the right adnexal area. Although there was no obvious endometrial-like echo in this mass, a 1.5×1.0×1.0 cm inhomogeneous zone with blood flow signal around was seen. Next to the right ovary, a 5.2×3.0×2.5 cm inhomogeneous hyperechoic mass with surrounding vascularity signal was noted (Figure 1). Fluid with a depth of about 2.5 cm was found in the pouch of Douglas. There were no obvious abnormalities in both kidneys, ureters and the bladder. Past and family history is not unusual.
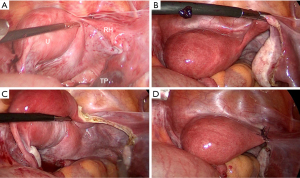
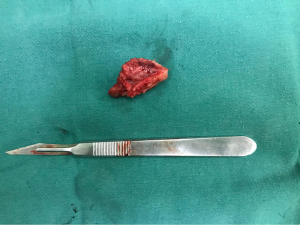
After being admitted due to suspected ectopic pregnancy with rudimentary horn, this patient chose a diagnostic laparoscopic exploration. During the operation, it was found that the ampulla of the right fallopian tube was enlarged to about 7.0×4.0 cm, with a purplish-blue surface. The right fallopian tube was connected to a muscular mass of about 5.0×1.5 cm, which had a right round ligament and was thought to be a rudimentary horn. This rudimentary horn was connected by a muscular band to the lower part of the uterus. A normal right ovary was observed next to the right tube. The uterus was situated towards the left. There was a normal adnexa and a round ligament on the left side of the uterus. Following the wishes of the patient and her family, we removed the fallopian tube and the rudimentary horn. Figure 2 shows the intraoperative findings and surgical procedures. We dissected the excised organ and found villous tissue in the fallopian tube and endometrial tissue in the rudimentary horn (Figure 3). Postoperative pathological examination also confirmed the presence of villous tissue in the tube and endometrial tissue in the uterus. The patient’s postoperative course was uneventful, and she left the hospital in good condition. A year later, the patient recovered well with mild dysmenorrhea and normal menstrual volume. Since the patient had no intention of becoming pregnant, contraceptive measures were taken.
Case 2
A 30-year-old female, G2P0, was first seen with amenorrhea for 7 weeks’ duration. She had no abnormal vaginal bleeding or abdominal pain. This patient’s menarche was at 13 years and experienced mild dysmenorrhea. She had a history of one artificial abortion. Past medical and social histories were unremarkable. Her right adnexal area was thickened with mild tenderness. Physical examination showed no other significant abnormalities. Her blood β-HCG was 10,277 mIU/mL. Transvaginal ultrasonography revealed that a 4.0×1.0×1.8 cm hypoechoic mass was connected to the right lateral wall of the uterus in the right adnexal area. No obvious endometrial-like echo was observed in this mass. A 1.4×1.3×1.4 cm hyperechoic mass with blood flow signal was observed close to the left ovary. A gestational sac was not found in the uterine endometrium. Fluid with a depth of about 2.0 cm was found in the pouch of Douglas. There were no obvious abnormalities in both kidneys, ureters and the bladder. Past and family history is not unusual.
Diagnostic laparoscopy revealed that the ampulla of the left tube was enlarged to about 3.0×3.0 cm, with a purplish-blue surface. The left ovary was normal. The right tube was connected to a mass of about 5.0×1.5 cm of muscular tissue, which had a right round ligament and was thought to be a rudimentary horn. This horn was connected by a fibrous strand band to the lower part of the uterus. A normal right ovary was noticed next to the right tube. The uterus was situated to the left. We performed salpingostomy and removed the rudimentary horn and the ipsilateral fallopian tube at the choice of the patient and her family. Postoperative pathological examination confirmed no endometrial tissue in the rudimentary horn. The patient was discharged from hospital as planned. Like case one, this patient recovered well without complications.
Discussion
The müllerian ducts are paired structures of mesodermal origin that fuse to create the uterus, cervix, and upper two-thirds of the vagina at approximately the 6th week of gestation. Normal development of müllerian ducts involves duct elongation, fusion, canalization, and septal resorption. Failure of these embryologic development can result in a variety of congenital uterine anomalies, one of which is unicornuate uterus with rudimentary horn. The etiology remains complex and uncertain, but chromosomes in most cases are normal, so these abnormalities are thought to be polygenic and multifactorial (4).
Unicornuate uterus can be further subdivided into four variants according to the American Fertility Society (2): (I) A1a communicating subtype, in which the endometrial cavity of a rudimentary horn is in open communication with the uterus; (II) A1b noncommunicating subtype, in which no open communication exists between endometrial cavity of a rudimentary horn and uterus; (III) A2 no-cavity subtype, in which the rudimentary horn does not have an endometrial cavity; and (IV) B no-horn subtype, in which no rudimentary horn is present. Embryologically, subtype B is the result of a complete atresia of Mullerian duct on one side. In such cases, ipsilateral fallopian tube is absent. In general, rudimentary horns (A1a, A1b and A2) are found in 74% of unicornuate uteri (2), and 70–90% of them are noncommunicating horns (A1b) (5,6).
Various imaging modalities are used to diagnose müllerian duct anomalies. The special shape of uterus and its cavity, and the connection between the muscular mass and the uterus is important for diagnosing this disease. Because of the fast, economical and non-radioactive characteristics, ultrasonography is frequently used in emergency or initial evaluations. For the diagnosis of müllerian duct anomalies, the transvaginal ultrasonography is superior to the transabdominal approach with an accuracy rate of 90–92% and 59%, respectively (7). In both cases reported here, the rudimentary horns were detected by transvaginal ultrasonography. Three-dimensional ultrasonography further increases the accuracy of diagnosis. The gold standard for diagnosing müllerian ducts anomalies is magnetic resonance imaging (MRI) which provides clear delineation of both the uterine cavity and its external contours. Hysterosalpingography is mainly used in infertility women to evaluate the uterine cavity and tubal patency; the test may indicate uterine anomaly but rarely provides a specific diagnosis. However, because the position of unicornuate uterus and rudimentary horn is changeable, the rudimentary horn is sometimes missed even with MRI, especially when it is very small, non-cavitated, or far from the uterus. Since development of the genital tract is closely related to the development of urinary tract, renal and ureteral abnormalities may occur simultaneously. About 40–60% of the müllerian duct anomalies present with renal abnormalities (5,8). However, the two cases we reported were not complicated with urinary system malformation.
Women who have a unicornuate uterus with a rudimentary horn have a higher incidence of gynecologic problems, including dysmenorrhea, chronic pelvic pain, infertility, abortions, torsion of rudimentary horn and ectopic pregnancies (5,9). The traditional view is that patients with functional, noncommunicating rudimentary horns often have progressive dysmenorrhea after menarche due to hematocele or endometriosis. Yet studies have found that only about 50% of patients have dysmenorrhea, which often begins in their 20 and 30 s (5). This may be due to hypoplastic endometrium and abnormalities of the endo-myometrial junction and arcuate arterioles that limit endometrium shedding and prevent hematometra (10). In the two cases we reported, one experienced mild dysmenorrhea and the other had no dysmenorrhea.
Ectopic pregnancy might occur in both fallopian tubes regardless of the subtype of rudimentary horn. Case 1 was A1a communicating subtype with tubal pregnancy located on the same side of the rudimentary horn, while case 2 was A1b noncommunicating subtype with tubal pregnancy in the contralateral side of rudimentary horn. Pokoly first reported a case of tubal pregnancy on the side of the noncommunicating rudiment horn (11), which had a corpus luteum at the contralateral side. Then Handa et al. reported a tubal pregnancy on the side of the noncommunicating rudimentary horn with the ipsilateral ovary carrying a corpus luteum (12). These findings showed that the fertilized ovum, or the sperm could migrate transperineally around the impregnating period. As a matter of fact, sperm transmigration occurs in approximately 50% of spontaneous human pregnancies, and ovum transmigration in approximately 40% (13).
For the same reason, fertilized ovum could implant in the cavity of both communicating or noncommunicating rudimentary horn. About 80–90% ectopic pregnancy in rudimentary horn results in a rupture during the second or third trimester due to poorly developed musculature, leading to life-threatening bleeding (6,14). The ultrasonography presents a gestational sac surrounded by myometrial tissue separate from the uterus and an empty uterine. Sometimes color Doppler ultrasonography reveals a vascular pedicle between the unicornuate uterus and the gestational sac in the rudimentary horn. Because rudimentary horn pregnancies are uncommon and fatal, doctors need to be familiar with their diagnostic criteria. As a routine obstetric ultrasonography, regional anatomy is required to rule out rudimentary horn pregnancy even when the gestational sac is located within the endometrial cavity and there is a normal myometrium surrounding the endometrium.
Although rare, torsion of rudimentary horn is documented. Wang reported a case of non-gravid rudimentary horn torsion where pregnancy existed in the unicornuate uterus in the second trimester (15). The torsion might be caused by changes in the position of rudimentary horn and the pregnant uterus. Compared with this case, torsion of the pregnant rudimentary horn cases was reported more (16,17).
Because the necessity of rudimentary horn resection was uncertain in the emergent situation of ectopic pregnancy hemorrhage, the rudimentary horn was left untouched in case reported by Handa et al. (12). This rudimentary horn was removed by laparoscopic surgery 8 months after the previous salpingectomy (12). It is worth discussing whether it is beneficial to remove the rudimentary horn simultaneously during tubal pregnancy operation. Due to abdominal pain and the major risk of pregnancy in the rudimentary horn, it is recommended to excise a cavitated uterine horn in women of reproductive age; this could be easily performed by laparoscopy, especially when the rudimentary horn is separated from the uterus. It is also expected that this removal would prevent torsion of the rudimentary horn and neoplastic diseases,from which even the non-lumen cornered uterus might benefit. The rudimentary horns were removed during laparoscopy of tubal pregnancy in both cases we reported. The patients’ postoperative course was uneventful, and they were discharged in good condition.
The limitation of this article is that it only included two cases. Since there are few literatures on ectopic pregnancy complicated with rudimentary horn, more case-control studies should be conducted to clarify the diagnostic and surgical issue on this topic.
To summarize, ectopic pregnancy might occur in both fallopian tubes regardless of the subtype of rudimentary horn. It is recommended to excise a cavitated rudimentary horn due to abdominal pain and the major risk of pregnancy in the rudimentary horn. It is also expected that this removal would prevent torsion of the rudimentary horn and neoplastic diseases, from which even the non-lumen rudimentary horn might benefit. Concomitant rudimentary horn excision and tubal pregnancy surgery might save the patients from re-operation.
Acknowledgments
Funding: This study was supported by Key Research and Development Programs of Science and Technology Bureau of Sichuan Province (Grant No. 2019YFS0421).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-43/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-43/coif). HC received a funding from Key Research and Development Programs of Science and Technology Bureau of Sichuan Province. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of West China Second University Hospital of Sichuan University [Approval No. 006(2020)]. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Byrne J, Nussbaum-Blask A, Taylor WS, et al. Prevalence of müllerian duct anomalies detected at ultrasound. Am J Med Genet 2000;94:9-12. [Crossref] [PubMed]
- Nahum GG. Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med 1998;43:877-87. [PubMed]
- Jurkovic D, Gruboeck K, Tailor A, et al. Ultrasound screening for congenital uterine anomalies. Br J Obstet Gynaecol 1997;104:1320-1. [Crossref] [PubMed]
- Rackow BW, Arici A. Reproductive performance of women with müllerian anomalies. Curr Opin Obstet Gynecol. 2007;19:229-37. [Crossref] [PubMed]
- Jayasinghe Y, Rane A, Stalewski H, et al. The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 2005;105:1456-67. [Crossref] [PubMed]
- Nahum GG. Rudimentary uterine horn pregnancy. The 20th-century worldwide experience of 588 cases. J Reprod Med 2002;47:151-63. [PubMed]
- Santos XM, Krishnamurthy R, Bercaw-Pratt JL, et al. The utility of ultrasound and magnetic resonance imaging versus surgery for the characterization of müllerian anomalies in the pediatric and adolescent population. J Pediatr Adolesc Gynecol 2012;25:181-4. [Crossref] [PubMed]
- Fedele L, Bianchi S, Agnoli B, et al. Urinary tract anomalies associated with unicornuate uterus. J Urol 1996;155:847-8. [Crossref] [PubMed]
- Thurber BW, Fleischer AC. Ultrasound features of rudimentary horn ectopic pregnancies. J Ultrasound Med 2019;38:1643-7. [Crossref] [PubMed]
- Fedele L, Marchini M, Baglioni A, et al. Endometrium of cavitary rudimentary horns in unicornuate uteri. Obstet Gynecol 1990;75:437-40. [PubMed]
- Pokoly TB. Ectopic pregnancy in a noncommunicating tube of a unicornuate uterus. A case report. J Reprod Med 1989;34:994-5. [PubMed]
- Handa Y, Hoshi N, Yamada H, et al. Tubal pregnancy in a unicornuate uterus with rudimentary horn: a case report. Fertil Steril 1999;72:354-6. [Crossref] [PubMed]
- Nahum GG, Stanislaw H, McMahon C. Preventing ectopic pregnancies: how often does transperitoneal transmigration of sperm occur in effecting human pregnancy? BJOG 2004;111:706-14. [Crossref] [PubMed]
- Siwatch S, Mehra R, Pandher DK, et al. Rudimentary horn pregnancy: a 10-year experience and review of literature. Arch Gynecol Obstet 2013;287:687-95. [Crossref] [PubMed]
- Wang B, Zhou JH, Jin HM. Torsion of a rudimentary uterine horn at 22 weeks of gestation. J Obstet Gynaecol Res 2011;37:919-20. [Crossref] [PubMed]
- Kumar N, Das V, Pandey A, et al. Torsion and rupture of a non-communicating rudimentary horn in a 17-week gestation in a 16-year-old girl: lessons learnt. BMJ Case Rep 2018;2018:bcr-2017-222073. [Crossref] [PubMed]
- Singh P, Gupta R, Das B, et al. Midtrimester spontaneous torsion of unruptured gravid rudimentary horn: presurgical diagnosis on magnetic resonance imaging. J Obstet Gynaecol Res 2015;41:1478-82. [Crossref] [PubMed]
Cite this article as: Chen H, Abeysundera E, Tian T, Qi X. Tubal pregnancy complicated with rudimentary horn: two case reports and literature review. Gynecol Pelvic Med 2022;5:20.