Mature cystic teratoma in Douglas’ pouch: a case report
Introduction
Mature cystic teratoma, also called dermoid cyst, arises from the germ cell arrested after the first meiotic division. They may contain any of the following three germ layers: ectoderm, mesoderm or endoderm. These layers typically form tissues that are foreign to the ovary and that have a disorganized structure and haphazard collection of tissues such as fat, hair, teeth and bone. Mature cystic teratoma occurs most commonly in the ovary and is one of the most common benign ovarian tumors, accounting for about 20% of ovarian tumors in adult (1,2). However, teratoma arises from extra-ovarian site is rare, and teratoma in the pouch of Douglas is extremely rare. Since the first case of mature cystic teratoma in pouch of Douglas was reported in 1978, only a few cases have been reported so far (3-6). Therefore, every case of teratoma in Douglas’ pouch is worth being reported, and this case-report adds one more case to the other cited studies. The exact etiology of extragonadal teratoma is unknown. The widely accepted theory is that extragonadal teratoma is automatically resected into the pouch of Douglas. In the present report, we presented a case of mature cystic teratoma in the pouch of Douglas successfully treated via single-port laparoscopic resection and discussed its etiology. We present the following case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-3/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
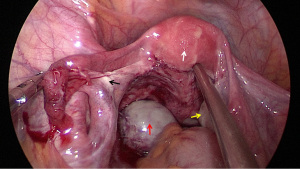
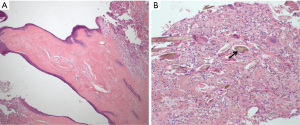
A 33-year-old female patient presented to our hospital with a two-month history of lower abdominal discomfort on December 20, 2021. Her general medical history revealed no diseases and surgery, and her general physical examination was normal. Gynecological examination showed there was a mass measuring about 5 cm in diameter in the pelvic cavity. Gynecological ultrasound revealed there was a cystic and solid mass measuring 5.97 cm × 3.86 cm × 5.67 cm in the left adnexal area (Figure 1). The tumor markers, including carbohydrate antigen-125 (CA-125), carbohydrate antigen 19-9 (CA 19-9), carcinoembryonic antigen and alphafetoprotein were all within normal range. The diagnosis of suspected ovarian teratoma was made, hence a single-port laparoscopic surgery was performed. Intraoperative findings showed a mass about 6 cm × 5 cm × 4 cm in size arising from the Douglas’ pouch. The mass was free from both ovaries and had membranous adhesion to the lateral pelvic wall and mesorectum (Figure 2). The uterus and the right ovary was normal in size and shape, but the left ovary was small considering the patient’s age (Figure 2). The mass was completely removed without rupture by single-port laparoscopy. Gross examination of the excised specimen revealed the tumor measuring 5 cm in diameter was grey-white and cystic and contained hair and fat. Histopathological findings showed the mass consisted of cyst lined by stratified squamous epithelium and multiple mature tissues such as fat and hair (Figure 3). No immature elements and ovarian tissues were found in the tumor. The tumor mass was diagnosed as a mature cystic teratoma by histological and immunohistochemical examination. These findings suggest that the mature cystic teratoma arised primarily from the pouch of Douglas. The patient had an uneventful recovery and was discharged after 2 days of postoperative hospitalization without any complications. It has been 3 months since the operation. The patient was followed up without any discomfort, and there were no abnormalities found by gynecological ultrasound.

Discussion
Mature cystic teratoma is one of the most common ovarian tumors. However, teratomas occurring at extragonadal sites are rare, and the most common extragonadal mature cystic teratomas are reported to be in the omentum (1,7,8). Teratomas originated from the pouch of Douglas are extremely rare. Only a few cases have been reported so far, since the first case of mature cystic teratoma in the pouch of Douglas was reported in 1978 (9). In the present report, we presented a case of mature cystic teratoma in pouch of Douglas resected without rupture by single-port laparoscopy.
Mature cystic teratoma in Douglas’ pouch has no specific clinical manifestation, and there may be some symptoms of abdominal distension or pain when the teratoma is large enough to cause abdominal discomfort. Therefore, it is difficult to make a definite diagnosis of teratoma in pouch of Douglas preoperatively, and majority of them are intraoperative incidental finding. Like ovarian mature cystic teratoma, mature cystic teratoma in the pouch of Douglas does not cause elevation of specific serum tumor markers. However, pelvic computed tomography (CT) or/and magnetic resonance imaging (MRI) can be helpful in preoperative diagnosis (10). Therefore, mature cystic teratoma in Douglas’ pouch is finally diagnosed by postoperative pathology.
As with ovarian mature cystic teratoma, the treatment for mature cystic teratoma in Douglas’ pouch is surgical removal. Laparoscopy is the preferred surgical modality (11). In recent years, with the development of minimally invasive surgery, laparo-endoscopic single-site surgery has been successfully applied. Single-port laparoscopy has a unique advantage in removing surgical specimen and can avoid tumor cell spread. Therefore, laparo-endoscopic single-site surgery is the first choice for the treatment of teratoma in our hospital. In our case, the tumor mass was successfully treated via single-port laparoscopic resection, and the patient had an enhanced and uneventful recovery after the laparo-endoscopic single-site surgery.
The etiology of extragonadal teratoma is considered to arise from early embryonic cell or primordial germ cell or totipotent cell (12). There are three theories that have been put forward to describe its etiology. The first theory is that extragonadal teratoma arises from an ectopic ovary, either due to inflammation such as pelvic inflammatory disease, or due to ovarian tissue implantation after surgery (4,10). The second theory is that extragonadal teratoma may be derived from displaced germ cell. In the early stage of fetal development, germ cell moves from the yolk sac to the genital ridge along the hindgut. During the migration, germ cell was trapped between the dorsal mesentery and the yolk sac endoderm, and eventually settled in the Douglas’ pouch (12). The third theory states that it is formed due to auto-amputation of an ovarian teratoma and its reimplantation into the Douglas’ pouch. Autoamputation theory was initially proposed by Thornton in 1881 (13). In our case, the third theory may better explain this extragonadal teratoma. Although no ovarian tissue was found in the postoperative pathology, the patient in this case had no history of abdominal surgery and pelvic inflammatory disease. Intraoperative findings revealed that the left ovary was small. Therefore, it seems that this extragonadal teratoma in our report was formed due to auto-amputation of the left ovarian teratoma and its reimplantation into the Douglas’ pouch.
This case report has some limitations. Firstly, no abdominal CT or MRI was performed before operation to fully evaluate the mass. Secondly, the transvaginal ultrasound of this patient did not provide the data of the bilateral ovarian size, and we naturally considered this mass to be a common ovarian teratoma before operation. Finally, there was no detailed available data on mature cystic teratoma in Douglas’ pouch in other similar case reports, so we did not make comparisons with other similar case reports, such as surgical modality, surgery time, blood loss and length of hospital stay, treatment outcome, etc.
In conclusion, we present an extremely rare case of mature cystic teratoma in Douglas’ pouch, which was successfully treated via single-port laparoscopic resection. Mature cystic teratoma in Douglas’ pouch is extremely rare, hence the clinical diagnosis may be a challenge. It may provide insights for the differential diagnosis of adnexal masses.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-3/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-3/coif). YS serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from May 2021 to April 2023. The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ohshima K, Umeda A, Hosoi A, et al. Mature Cystic Teratoma in Douglas' Pouch. Case Rep Pathol 2015;2015:202853. [Crossref] [PubMed]
- Talerman A, Vang R. Germ cell tumors of the ovary. In: Kurman RJ. editor. Blaustein’s Pathology of the Female Genital Tract. 5th edition. New York, NY, USA: Springer, 2008:967-1033.
- Matsushita H, Kurabayashi T, Yanase T, et al. Autoamputation of an ovarian cyst: a case report. J Reprod Med 2009;54:709-11. [PubMed]
- Kusaka M, Mikuni M. Ectopic ovary: a case of autoamputated ovary with mature cystic teratoma into the cul-de-sac. J Obstet Gynaecol Res 2007;33:368-70. [Crossref] [PubMed]
- Peitsidou A, Peitsidis P, Goumalatsos N, et al. Diagnosis of an autoamputated ovary with dermoid cyst during a Cesarean section. Fertil Steril 2009;91:1294.e9-12. [Crossref] [PubMed]
- Bartlett CE, Khan A, Pisal N. Parasitic dermoid cyst managed laparoscopically in a 29-year-old woman: a case report. J Med Case Rep 2009;3:63. [Crossref] [PubMed]
- Wani BN, Rathod V, Banode P, et al. An omental teratoma in a young girl. Clin Pract 2011;1:e129. [Crossref] [PubMed]
- Hegde P. Extragonadal omental teratoma: a case report. J Obstet Gynaecol Res 2014;40:618-21. [Crossref] [PubMed]
- Lefkowitch JH, Fenoglio CM, Richart RM. Benign cystic teratoma of the retrouterine pouch of Douglas. Am J Obstet Gynecol 1978;131:818-20. [Crossref] [PubMed]
- Sethi P, Purkait S. Mature Cystic Teratoma of Douglas' Pouch: A Rare Entity. Cureus 2019;11:e5515. [Crossref] [PubMed]
- Medeiros LR, Stein AT, Fachel J, et al. Laparoscopy versus laparotomy for benign ovarian tumor: a systematic review and meta-analysis. Int J Gynecol Cancer 2008;18:387-99. [Crossref] [PubMed]
- Oosterhuis JW, Stoop H, Honecker F, et al. Why human extragonadal germ cell tumours occur in the midline of the body: old concepts, new perspectives. Int J Androl 2007;30:256-63; discussion 263-4. [Crossref] [PubMed]
- Thornton KD. Dermoid cyst. Am J Obstet 1881;19:697.
Cite this article as: Deng J, Shen Y, Chen J, Guo X, Xie C. Mature cystic teratoma in Douglas’ pouch: a case report. Gynecol Pelvic Med 2022;5:31.