
Retroperitoneal malignant perivascular epithelioid cell tumor: a rare case report and literature review
Introduction
Perivasuclar epithelioid cell tumor (PEComa) is a rare group of mesenchymal tumors with unique histological and immunophenotypes, which was first proposed by Zamboni in 1996 (1). PEComa can be occured in any ages, mostly in the middle-age. The lesions can involve in various parts of bodies, and uterus is the most common organ (2,3). Retroperitoneal PEComas are extremely rarely seen and almost all benign lesions (2,3).
Herein, we present a case of malignant retroperitoneal PEComa with literature review to draw attention to this disease. Based on a literature review in PubMed and Web of Science with the terms of (“malignant perivascular epithelioid cell tumor” or “malignant PEComa”) and (“Post-peritoneal” or “retroperitoneal”), similar report of retroperitoneal malignant PEComa in this paper was rare reported before, especially the one from China (4,5). Compared with former cases, we focused on histological and immunohistochemical (IHC) characteristics of the tumor, follow-up and long-term outcome. We present the following case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-44/rc).
Case description
A 27-year-old Chinese female patient, gravida 0 para 0, was admitted to our hospital with a chief complain of chronical abdominal pain in Jan. 20, 2019. This symptom had occurred over a period of 3 months. She refused any medical and family history. Physical examination presented that the patient got an adnexal mass. Remaining physical examination did not reveal any additional abnormalities. Trans-vaginal ultrasound revealed a neoplasm of size 15 cm × 8 cm × 10 cm in the right adnexal region. The serum tumor markers were normal. The medical history and family history was normal. With a suspicion of ovarian cyst, a surgery then arranged.
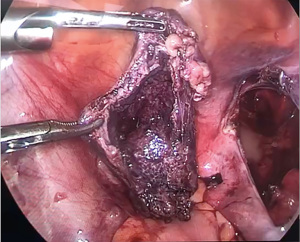
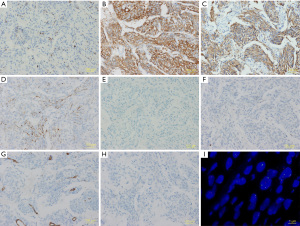
At the explorative laparoscopic, the right ovary is atrophied of 2 cm × 2 cm × 2 cm in size; and the left ovary and uterus were normal in size. The rest exploration of pelvic and abdomen was normal. A retroperitoneal mass was noticed, with 12 cm × 10 cm × 10 cm in size. Following laparoscopy confirmed the mass with multilocular cyst retroperitoneal, adhesion to the right ureter and iliac vessels, and the boundary is unclear, containing about 500 mL turbid fluid (Figure 1). Subsequent IHC staining indicated HMB-45 (26% positive) (Figure 2A), SMA (82% positive) (Figure 2B), Caldesmon (78% positive) (Figure 2C), Desmin (27% positive) (Figure 2D), Ki-67 (25% positive), ER (15% positive), PR (12% positive), CDK-4 (5% positive), MiTF (5% positive), S-100 (negative) (Figure 2E), CD117 (negative) (Figure 2F), CD34 (negative) (Figure 2G), EMA (negative) (Figure 2H), MDM2 (negative), WT-1 (negative) and fluorescence in situ hybridization (FISH) test revealed negative with MDM2 gene (Figure 2I). There was no existence of necrosis in the mass.
After a clinic-pathological debate, the patient was diagnosed with retroperitoneal malignant PEComa. Three months later of the treatment, the patient returned for follow-up and trans-vaginal ultrasound revealed with ascites. The second review was undertaken at six months later of the surgery, and no ascites was detected. And then, she received another 3 follow-ups every 6 months. During the 2 years post-surgery, the patient recovered well without any chemotherapy, radiation therapy, or other drug interventions. The patient claimed she was quite satisfied with the treatment and the prognosis she received.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Origin of PEComa
In 1991, Pea first reported that renal angiomyolipoma commonly expressed HMB-45, a relatively specific marker of melanocyte-differentiated tumors (6). In 1992, Bonetti proposed the concept of “perivascular epithelial cells” to name these cells (7). In 1994, Bonetti further unified the constitutive cells of angiomyolipoma, lung clear cell “sugar” tumor, and lymphangiomyomatosis as “perivascular epithelioid cells”, which are characterized with “unique muscle cells, different expressions of Melanoma-associated antigen” (8). In 1996, Zamboni et al. firstly used the term of PEComa to describe a pancreas-derived clear epithelioid cell tumor with HMB-45 (+) (1).
In the following years, some reports on PEComa satisfied these basic histological features, and those tumors extensively distributed in bodies. Nowadays, based on the definition of the World Health Organization tumor classifications, PEComa refers to an interstitial tumor composed of perivascular epithelioid tissue with histological and immunohistochemical features (9). Angiomyolipoma, lymphangioleiomyoma, and clear-cell sugar tumor of the lung are typical members of the PEComa family (7,8,10,11).
Pathological characteristics
Most patients have no obvious symptoms. Some can only accompany with abdominal pain, abdominal distension and diarrhea. PEComa is mostly benign. Due to the reports were limited, the diagnostic criteria for malignant PEComa have not been establishment. Folpe et al. classified PEComa tumors as benign, uncertain malignant potential and malignant (12).
- Benign: tumor diameter <5 cm, non-infiltrative, mild nuclear grade and cellularity, mitotic index ≤1/50 high power fields (HPF), no necrosis and vascular invasion.
- Uncertain malignant potential (nuclear pleomorphism/multinucleated giant cells only or tumor diameter >5 cm only).
- Malignant: tumor diameter >5 cm, infiltrative, high nuclear grade and cellularity, mitotic rate ≥1/HPF, necrosis and vascular invasion).
Grossly, the interior surface is yellowish to grayish red and the boundary is unclear, with or without focal hemorrhage and necrosis.
Under the microscope, PEComa is often located around the blood vessels, and the cells are arranged around the lumen of the blood vessel. Typical perivascular epithelioid cells are epithelial-like cells around the vicinity of the blood vessels, and the fusiform cells tend to be far from the blood vessels. In the uterus, kidney, perirenal or peritoneum, PEComa cells can exhibit a large number of interstitial transparency (7,8,11). In immunohistochemistry, nearly 100% of PEComas expressed HMB-45 and the positive rate of SMA was 59%, Melan-A was 41%, CD117 was 33%, Desmin was 31%, S-100 was 10%, and negative of cytokeratins (12).
Antidiastole
Malignant melanoma
Due to the strong positive expression of HMB-45, PEComa is easily misdiagnosed as malignant melanoma. In malignant melanoma immunohistochemistry, HMB-45 and S-100 expression are positive, and SMA expression is negative. However, in PEComa, SMA expression is generally positive, and S-100 expression is negative or rarely positive (3).
Epithelioid leiomyoma
The expression of SMA in epithelioid leiomyoma is nearly 100% positive, and the expression of HMB-45 is often negative, while HMB-45 expression in PEComa is diffuse positive strongly (13).
Clear cell carcinoma
Clear cell carcinoma lacks of the perivascular epithelial-like cell; keratin and carcinoembryonic antigen expressions are positive; while HMB-45 and SMA expressions are negative (3).
Endometrial stromal sarcoma
The CD10 expression of endometrial stromal sarcoma is diffusely strong, while the CD10 expression of PEComa is negative. In addition, PEComa was positive for both HMB45 and Melan-A expressions (13,14).
Treatment and follow-up
Surgical resection is still the most reliable and effective treatment currently, including removal of primary and metastatic lesions. The roles of chemotherapy and immunotherapy are still unclear. Although most PEComas are benign, the biological behavior is not clear, and may accompany with potential behaviors, thus a long-term follow-up is recommended.
Strengths and limitations
In this case, we preformed enough immunohistochemistry stains to reach the final diagnosis and presented antidiastole characteristics. Some previous literature revealed 18F-FDG-PET/CT can help characterize these lesions and new therapies with inhibitory m-TOR may open a hopeful therapeutic window (15). But we failed to get the PET/CT scan and immune therapy, due to the patient was lack of insurance and cannot afford it herself.
Conclusions
Retroperitoneal malignant PEComa was rare reported before. Specially attention should be paid to the retroperitoneal malignant PEComa. For take home massage, immunohistochemistry stain is strongly recommended for the diagnosis of PEComa. A surgical removement of the mass is the main treatment method. The roles of chemotherapy and immunotherapy are still unclear and a long-term follow-up is suggested. However, with limited clinical and follow-up data, further cases need to be collected.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-44/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-44/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zamboni G, Pea M, Martignoni G, et al. Clear cell "sugar" tumor of the pancreas. A novel member of the family of lesions characterized by the presence of perivascular epithelioid cells. Am J Surg Pathol 1996;20:722-30. [Crossref] [PubMed]
- Folpe AL. Neoplasms with perivascular epithelioid cell differentiation (PEComas). In: Fletcher CDM, Unni KK, Mertens F. editors. Pathology and genetics of tumours of soft tissue and bone. Lyon, France: IARC Press; 2002:221-2.
- Hornick JL, Fletcher CD. PEComa: what do we know so far? Histopathology 2006;48:75-82. [Crossref] [PubMed]
- Bleeker JS, Quevedo JF, Folpe AL. "Malignant" perivascular epithelioid cell neoplasm: risk stratification and treatment strategies. Sarcoma 2012;2012:541626. [Crossref] [PubMed]
- Touloumis Z, Giannakou N, Sioros C, et al. Retroperitoneal perivascular epithelioid cell tumours: A case report and review of literature. World J Clin Cases 2019;7:3524-34. [Crossref] [PubMed]
- Pea M, Bonetti F, Zamboni G, et al. Melanocyte-marker-HMB-45 is regularly expressed in angiomyolipoma of the kidney. Pathology 1991;23:185-8. [Crossref] [PubMed]
- Bonetti F, Pea M, Martignoni G, et al. PEC and sugar. Am J Surg Pathol 1992;16:307-8. [Crossref] [PubMed]
- Bonetti F, Pea M, Martignoni G, et al. Clear cell ("sugar") tumor of the lung is a lesion strictly related to angiomyolipoma--the concept of a family of lesions characterized by the presence of the perivascular epithelioid cells (PEC). Pathology 1994;26:230-6. [Crossref] [PubMed]
- Fletcher C. Pathology and genetics of tumors of soft tissue and bone. World Health Organization Classification of Tumors 2002;4:35-46.
- Mizuuchi Y, Nishihara K, Hayashi A, et al. Perivascular epithelial cell tumor (PEComa) of the pancreas: a case report and review of previous literatures. Surg Case Rep 2016;2:59. [Crossref] [PubMed]
- Martignoni G, Pea M, Reghellin D, et al. PEComas: the past, the present and the future. Virchows Arch 2008;452:119-32. [Crossref] [PubMed]
- Folpe AL, Mentzel T, Lehr HA, et al. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol 2005;29:1558-75. [Crossref] [PubMed]
- Silva EG, Deavers MT, Bodurka DC, et al. Uterine epithelioid leiomyosarcomas with clear cells: reactivity with HMB-45 and the concept of PEComa. Am J Surg Pathol 2004;28:244-9. [Crossref] [PubMed]
- Lehman NL. Malignant PEComa of the skull base. Am J Surg Pathol 2004;28:1230-2. [Crossref] [PubMed]
- Nicolás I, Fusté P, Saco A, et al. Perivascular epitheliod cell tumors: Study of three gynecological cases. Med Clin (Barc) 2019;153:83-7. [Crossref] [PubMed]
Cite this article as: Zeng X, Li JK. Retroperitoneal malignant perivascular epithelioid cell tumor: a rare case report and literature review. Gynecol Pelvic Med 2022;5:28.


