
Laparoscopic and hysteroscopic discovery of intrauterine fallopian tube incarceration after dilatation and curettage: a case report and review of the literature
Introduction
Dilation and curettage (D&C) is the most commonly performed gynecological procedure, and uterine perforation is one of the most common severe complications (1). Many perforations are undetected during intrauterine procedures. A minority of perforations may accompany intestinal injuries or active bleeding, which require surgery. Previous reports have described the small intestine, appendix, omentum, fallopian tube or ovary entering the uterine cavity due to uterine perforation (1-4). Patients may have painful symptoms such as the typical triad of abdominal pain, abnormal vaginal discharge, and dyspareunia, or amenorrhea occasionally. We here report a 32-year-old woman admitted to our department due to an ovarian mass and intrauterine mass without any obvious symptoms, who was found to have fallopian tube incarceration caused by a D&C. We present the following case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-1/rc).
Case presentation
In April 2019, a 32-year-old woman presented to our department complaining of mild pain in the lower left abdominal quadrant for 3 years. The patient underwent D&C of the uterine cavity one month after term delivery due to space-occupying lesions 3 years ago. After surgery, she had mild abdominal pain when walking for a long distance or when carrying heavy weights. She did not have fever, menometrorrhagia, dysmenorrhea, vaginal discharge, or dyspareunia. There was no relevant personal and family history. Physical examination showed that the patient was in good general condition. Her vital signs were stable, and no other abnormalities were found. Gynecologic examination revealed a left adnexal cystic mass approximately 4 cm in size, mobile, well-bounded with tenderness. Blood analysis revealed a normal leukocyte count. Serum tumor markers were all negative. Transvaginal ultrasound showed a cystic mass of about 4 cm on the left side of the ovary suspected to be an ovarian endometriosis cyst and endometrial polyps in the cavity (Figure 1).
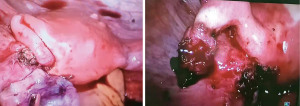
Hysteroscopy was performed first, and showed a mass on the left side of the uterine wall provisionally identified as polyps, blocking the left orifice of the fallopian tube similar to the hysteroscopic view in the case report by Ceccaldi (5). This was mistakenly thought to be a polyp and was removed. However, after removal of the polyp-like mass, a similar mass appeared at the same location. Laparoscopy confirmed intrauterine incarceration of the left fallopian tube from the uterine fundus. In addition, a left ovarian mass which was full of chocolate-colored fluid with a smooth capsule was suspended without adhesion to the surrounding tissues. The fallopian tube was carefully pulled out of the uterus and both salpingectomy and oophorocystectomy were performed after informed consent was obtained again from her husband. Finally, the uterine wall defect and ovary were repaired with Monocryl sutures (Figure 2). The patient recovered quickly after operation, and was discharged 2 days after operation without any adverse or unanticipated events.
The pathological report confirmed that the intrauterine mass contained tubal epithelium due to incarceration of the fallopian tube, and the left ovarian cyst was the result of endometriosis. After surgery, the patient’s pain was totally resolved. The patient received three cycles of gonadotropin-releasing hormone agonist therapy. The patient shows no signs of relapse of endometriosis, till January 2022.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Uterine perforation is extremely rare after D&C. The incidence of uterine perforation during the first trimester termination of pregnancy has been estimated to be 0.8–6.4/1,000 procedures. However, the incidence rate cannot be accurately estimated as most uterine perforations are successfully treated conservatively and not reported. Furthermore, many perforations are undetected. Kaali found that uterine perforation occurred in 14/707 (19.8/1,000 procedures) of first trimester elective abortions, where direct visualization was employed at the time of the procedure (6),
which is at least three times higher than the incidence previously mentioned. Uterine perforations are usually diagnosed as a result of physician’s suspicion. Definite diagnosis can be made on rare occasions when abdominal contents are found in the cervix or instruments can reach beyond the cavity during intrauterine procedures. When uterine perforations are accompanied by active bleeding or intestinal injuries, surgery should be considered. However, most uterine perforations heal themselves. Only a few patients develop symptoms if uterine perforations are not identified quickly, which are always complicated with tissue incarceration. Incarcerated tissues may include the intestine, omentum, fallopian tube, or even the ovary. Patients may have painful symptoms such as the typical triad of abdominal pain, abnormal vaginal discharge, and dyspareunia, or amenorrhea occasionally (7). As the symptoms and the accessory examinations are not typical, clinical diagnosis is still difficult. Definite diagnosis can only be made during surgery with laparotomy, laparoscopy or hysteroscopy.
In 1978, Steigrad first reported intrauterine fallopian tube incarceration (8). Since then, a total of 20 cases of fallopian tube incarceration have been reported (Table 1). All of them were caused by D&C. Five cases received D&C due to retained placenta or postpartum hemorrhage after delivery, 12 for first trimester pregnancy, 1 for second trimester pregnancy, and the remaining 2 patients received surgical abortion without specific gestational age. Only 2 of these cases were diagnosed quickly and underwent emergency surgery due to postpartum hemorrhage and suspected appendix injury (9,19). The others had abnormal vaginal discharge, vaginal bleeding, dyspareunia, dysmenorrhea, menometrorrhagia, amenorrhea, pelvic or abdominal pain, secondary fertility or even ectopic pregnancy (18). A few cases developed a tender uterus or cervical motion tenderness, whereas most were asymptomatic. With regard to accessory examinations, transvaginal ultrasound usually revealed a mass in the uterine cavity misdiagnosed as an endometrial polyp or submucous leiomyoma. Furthermore, magnetic resonance imaging and hysterosalpingography may contribute to the diagnosis of intrauterine fallopian tube incarceration. Most commonly, hysteroscopy and laparoscopy were used. In some emergent situations or where there is a lack of surgical expertise, laparotomy may be necessary. Salpingectomy or salpingoplasty can be selected depending on the anatomy and patients’ pregnancy wishes. However, the fallopian tube in four cases was resected before choices could be made due to misdiagnosis (7-10). Two patients delivered successfully via cesarean section and one was still pregnant without any related complications in the second trimester (5,14,22).
Table 1
| N | Author | Year | Age (years) | Time from D&C | Reasons for D&C | Symptoms | Pelvic examination | Accessory examination | Treatment | Fallopian tube | Conception |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Steigrad et al. (8) | 1978 | 26 | 10 months | Postpartum hemorrhage after delivery | Abnormal vaginal discharge, vaginal bleeding, dyspareunia | A polypoidal mass passing through the cervix into the vagina | n/a | Twisted away and then laparotomy | Twisted away from vagina | Sterilized |
| 2 | Lapas et al. (9) | 1987 | 38 | Immediately | n/a | n/a | n/a | n/a | Emergency laparotomy | Already removed during D&C | n/a |
| 3 | Thomas (10) | 2003 | 36 | 6 months | First-trimester pregnancy | Dysmenorrhea, menometrorrhagia, lower back pain | Not specific | Ultrasound | Hysteroscopy | Salpingectomy | n/a |
| 4 | Deffieux et al. (11) | 2008 | 34 | 5 years | First-trimester pregnancy | Pelvic pain | Not specific | MRI | Laparoscopy, hysteroscopy | Salpingectomy | n/a |
| 5 | Alanbay et al. (12) | 2009 | 28 | 2 years | First-trimester pregnancy | Secondary infertility | Not specific | Hysterosalpingography, ultrasound | Laparoscopy, hysteroscopy, mini-laparotomy | Preserved | n/a |
| 6 | Trio et al. (13) | 2010 | 31 | 4 days | First-trimester pregnancy | Abdominal pain, vaginal bleeding | n/a | Ultrasound | Laparoscopy | Preserved | n/a |
| 7 | Ceccaldi et al. (5) | 2011 | 33 | 18 months | n/a | Secondary infertility | n/a | Hysterosalpingography | Laparoscopy, hysteroscopy | Preserved | Pregnant in the second trimester |
| 8 | Damiani et al. (7) | 2011 | 25 | 18 months | First-trimester pregnancy | Pelvic pain, dyspareunia, nausea, vomiting, diarrhea, vaginal bleeding, abnormal vaginal discharge | Tender uterus | Ultrasound | Hysteroscopy | Removed by forceps | n/a |
| 9 | Damiani et al. (7) | 2011 | 30 | 3 months | Postpartum hemorrhage after delivery | Amenorrhea | Not specific | Ultrasound | Hysteroscopy, laparoscopy | Salpingectomy | n/a |
| 10 | Cremieu et al. (14) | 2012 | 28 | n/a | First-trimester pregnancy | Secondary infertility | Not specific | Hysterosalpingography | Laparoscopy | Preserved | Cesarean section at term |
| 11 | Kondo et al. (15) | 2013 | 22 | 11 months | Retained placenta and postpartum hemorrhage after delivery | Pelvic pain, amenorrhea | Tender uterus | Ultrasound and MRI | Laparoscopy | Salpingectomy | n/a |
| 12 | Guzel et al. (16) | 2014 | 25 | 3 years | First-trimester pregnancy | Secondary infertility | Not specific | Ultrasound | Laparoscopy, hysteroscopy | Preserved | n/a |
| 13 | Nkwabong et al. (17) | 2014 | 36 | n/a | First-trimester pregnancy | Abdominal pain, vaginal bleeding | Tender uterus | n/a | Laparotomy | Salpingectomy | n/a |
| 14 | Lin et al. (18) | 2015 | 39 | 6 years | First-trimester pregnancy | Vaginal bleeding, ectopic pregnancy | Tenderness in the right adnexa | Serum HCG positive | Laparoscopy, hysteroscopy | Salpingectomy | n/a |
| 15 | Dean et al. (19) | 2017 | 31 | Immediately | Second-trimester pregnancy | Postpartum hemorrhage | Not specific | Ultrasound | Laparoscopy | Preserved | n/a |
| 16 | Boujenah et al. (20) | 2017 | 33 | 9 months | Retained placenta after delivery | Abdominal pain, spotting and amenorrhea | Not specific | 3D endovaginal ultrasound | Laparoscopy, hysteroscopy | Salpingectomy | n/a |
| 17 | Camus et al. (21) | 2019 | 29 | 9 months | First-trimester pregnancy | Abnormal vaginal discharge | Not specific | Ultrasound and MRI | Laparoscopy, hysteroscopy | Preserved | n/a |
| 18 | Boughizane et al. (22) | 2020 | 22 | 2 years | First-trimester pregnancy | Secondary infertility | Not specific | Ultrasound and hysterosalpingography | Laparoscopy, hysteroscopy | Preserved | Cesarean section at term |
| 19 | Sedrati et al. (23) | 2021 | 33 | 6 months | First-trimester pregnancy | Pelvic pain | Cervical motion tenderness | Ultrasound | Laparoscopy, hysteroscopy | Salpingectomy | n/a |
| 20 | Shu et al. (24) | 2022 | n/a | 2 months | Retained placenta after delivery | Pelvic pain | Not specific | MRI, diagnostic hysteroscopy and laparoscopy | A robotic surgical platform | Salpingectomy | n/a |
| 21 | Present case | 2022 | 32 | 3 years | Retained placenta after delivery | Mild abdominal pain | Not specific | Ultrasound | Laparoscopy, hysteroscopy | Salpingectomy | n/a |
MRI, magnetic resonance imaging; n/a, not available; D&C, dilatation and curettage; HCG, human chorion gonadotropin.
According to the cases above, we can see that the history of intrauterine operation is necessary for the diagnosis of intrauterine fallopian tube incarceration. The most commonly differential diagnoses are endometrial polyp and submucous leiomyoma which are showed by the transvaginal ultrasound. Sometimes it may be misdiagnosed as uterine vascular lesions which can be ruled out by the ultrasound with colour Doppler (20). Advanced examinations of magnetic resonance imaging and hysterosalpingography can be helpful for the diagnosis. However, hysteroscopy and laparoscopy are needed to make a definite diagnosis and treatment.
Our patient was the 21st case of intrauterine fallopian tube incarceration. There are several learning points from our case. Firstly, most severe perforations are diagnosed quickly. Delayed presentation of uterine perforation is extremely rare. In this case, after reviewing her history, we confirmed that the intrauterine fallopian tube incarceration was caused by D&C. The use of ultrasound guidance during surgical termination can reduce the complications related to D&C (16). Secondly, the pain in our patient was ignored by herself and the doctor because of the mild degree of pain and without any other complications related. The fallopian tube incarceration was found coincidentally. If this patient did not have an intrauterine mass or an ovarian mass, the incarceration would not have been identified, which may be present for the rest of her life. We first performed hysteroscopy but did not recognize the fimbriae of the fallopian tube and removed the fimbriae. If we had suspected the mass to be fallopian tube fimbriae and did not remove it, or we had performed laparoscopy first, salpingectomy could have been avoided as shown in the report by Boughizane et al. and Camus et al. (21,22).
Conclusions
Intrauterine fallopian tube incarceration is a rare complication of D&C which occurred after uterine perforation and may show only ambiguous symptoms. Care should be taken to recognize uterine perforation when performing D&C and differential diagnosis should be considered.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-1/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-1/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Su S, Tao G, Dong B, et al. Delayed presentation of uterine perforation with ovary migration after dilatation and curettage. Int J Clin Exp Med 2015;8:6311-4. [PubMed]
- Augustin G, Majerović M, Luetić T. Uterine perforation as a complication of surgical abortion causing small bowel obstruction: a review. Arch Gynecol Obstet 2013;288:311-23. [Crossref] [PubMed]
- Dignac A, Novellas S, Fournol M, et al. Incarceration of the appendix complicating a uterine perforation following surgical abortion: CT aspects. Emerg Radiol 2008;15:267-9. [Crossref] [PubMed]
- Koshiba A, Koshiba H, Noguchi T, et al. Uterine perforation with omentum incarceration after dilatation and evacuation/curettage: magnetic resonance imaging findings. Arch Gynecol Obstet 2012;285:887-90. [Crossref] [PubMed]
- Ceccaldi PF, Nguyen T, Mandelbrot L. Unusual synechia at hysterosalpingography: intrauterine fallopian tube after surgical abortion. Fertil Steril 2011;95:2078-9. [Crossref] [PubMed]
- Kaali SG, Szigetvari IA, Bartfai GS. The frequency and management of uterine perforations during first-trimester abortions. Am J Obstet Gynecol 1989;161:406-8. [Crossref] [PubMed]
- Damiani GR, Tartagni M, Crescini C, et al. Intussusception and incarceration of a fallopian tube: report of 2 atypical cases, with differential considerations, clinical evaluation, and current management strategies. J Minim Invasive Gynecol 2011;18:246-9. [Crossref] [PubMed]
- Steigrad SJ, Margin CJ. Fallopian tube presenting as a uterine polyp. Aust N Z J Obstet Gynaecol 1978;18:281-3. [Crossref] [PubMed]
- Lapas KA, Todorov I. Rare case of amputation of the right tube during therapeutic abortion by the vacuum aspiration method. Akush Ginekol (Sofiia) 1987;26:75-6. [PubMed]
- Thomas PC. Intussusception of a fallopian tube after dilatation and curettage. Aust N Z J Obstet Gynaecol 2003;43:169-70. [Crossref] [PubMed]
- Deffieux X, Kane A, Faivre E, et al. Intrauterine fallopian tube incarceration: an uncommon complication of termination of pregnancy by vacuum aspiration. Fertil Steril 2008;90:1938-9. [Crossref] [PubMed]
- Alanbay I, Dede M, Karaşahin E, et al. Herniation of fallopian tube through perforated uterine wall during previous first trimester surgical abortion in an infertile patient. J Obstet Gynaecol Res 2009;35:997-9. [Crossref] [PubMed]
- Trio C, Recalcati D, Sina F, et al. Intrauterine fallopian tube incarceration after vacuum aspiration for pregnancy termination. Int J Gynaecol Obstet 2010;108:157-8. [Crossref] [PubMed]
- Cremieu H, Rubod C, Oukacha N, et al. About two cases of intra-uterine incarceration post-vacuum aspiration: diagnosis and management. J Gynecol Obstet Biol Reprod (Paris) 2012;41:387-92. [Crossref] [PubMed]
- Kondo W, Bruns RF, Nicola MC, et al. Laparoscopic treatment of intrauterine fallopian tube incarceration. Case Rep Obstet Gynecol 2013;2013:205957. [Crossref] [PubMed]
- Guzel AB, Kucukgoz Gulec U, Toksoz L, et al. Unusual complication of 1st-trimester surgical abortion in patient with a septate uterus: intrauterine fallopian tube herniation. J Obstet Gynaecol 2014;34:200. [Crossref] [PubMed]
- Nkwabong E, Ourtchingh C, Mvondo T. An induced abortion complicated by fallopian tube incarceration in the uterine cavity. J Obstet Gynaecol India 2014;64:32-3. [Crossref] [PubMed]
- Lin F, Yue DX, Quinn MJ, et al. Ectopic pregnancy in an incarcerated fallopian tube. Am J Obstet Gynecol 2015;213:244.e1-2. [Crossref] [PubMed]
- Dean M, Stamatopoulos N, Vancaillie T. A severed IP ligament as a cause for trans-vaginal uterine bleeding post termination of pregnancy: a case report. Pan Afr Med J 2017;27:95. [Crossref] [PubMed]
- Boujenah J, Benoit B, Djafer R, et al. Intrauterine fallopian tube intussusception after vacuum aspiration: Sonographic features and differential diagnosis. Eur J Obstet Gynecol Reprod Biol 2017;216:264-6. [Crossref] [PubMed]
- Camus MF, Chauvet P, Hordonneau C, et al. Laparoscopic Management of an Intrauterine Fallopian Tube Incarceration After Curettage for a Non-progressing Pregnancy. J Minim Invasive Gynecol 2019;26:805. [Crossref] [PubMed]
- Boughizane S, Bannour B, Rjiba G, et al. Intrauterine Fallopian Tube Incarceration After Vacuum Aspiration for Pregnancy Termination Causes Infertility. J Minim Invasive Gynecol 2020;27:254-5. [Crossref] [PubMed]
- Sedrati A, Alonso L, Wagner S, et al. Fallopian Tube Prolapse Through the Internal Cervical os: A Rare Complication of Uterine Perforation. J Minim Invasive Gynecol 2021;28:1808-9. [Crossref] [PubMed]
- Shu M, Nassar D, Chun CY, et al. Intrauterine Fallopian Tube Incarceration after Suction Curettage with Uterine Perforation. J Minim Invasive Gynecol 2022;29:457-9. [Crossref] [PubMed]
Cite this article as: Wang Q, Qi X, Zhou X. Laparoscopic and hysteroscopic discovery of intrauterine fallopian tube incarceration after dilatation and curettage: a case report and review of the literature. Gynecol Pelvic Med 2022;5:34.



